28 May 2022: Clinical Research
Modified Posterolateral Approach for the Treatment of 2-Part Fractures of the Posterior Malleolus Associated with Medial and Lateral Malleolar Fractures: 1 Incision, 2 Windows, 3 Steel Plates
Yanqing Gu1AG, Lei Zhao1B, Yan Ren1C, Yang Wang1D, Chenyang Xu1C, Chunzhi Jiang1CDF*DOI: 10.12659/MSM.936039
Med Sci Monit 2022; 28:e936039
Abstract
BACKGROUND: The aim of this study was to investigate the effect of the modified posterolateral approach using 1 incision, 2 windows, and 3 plates in the treatment of 2-part posterior malleolus fractures complicated with medial and lateral malleolus fractures.
MATERIAL AND METHODS: Twelve patients with 2-part fractures of the posterior malleolus complicated with medial and lateral malleolar fractures and treated by the modified posterolateral approach from January 2018 to January 2021 were studied retrospectively. After surgery, the ankle hindfoot score and visual analog scale (VAS) of the American Orthopedic Foot and Ankle Society (AOFAS) were used for evaluation.
RESULTS: The average follow-up time of the 12 patients was 18 months (7-30 months). All patients had no infection, and their incisions healed in the first stage. Postoperative radiography showed that the average fracture healing time was 12.5 weeks (10-15 weeks). The average time for patients to walk weight bearing was 13 weeks (11-16 weeks), and there was no obvious pain or discomfort. At the last follow-up, the average AOFAS ankle hindfoot score of the 12 patients was 87.5 (77-95), with 7 excellent and 5 good scores. The VAS score improved from before surgery (average 8.25 points) to after surgery (average 1 point). The curative effect was satisfactory.
CONCLUSIONS: The posterolateral approach using 1 incision, 2 windows, and 3 steel plates was effective in the treatment of 2-part posterior malleolus fractures complicated with medial and lateral malleolus fractures.
Keywords: ankle fractures, Fractures, Bone, Fractures, Cartilage, Fractures, Closed, Fracture Fixation, Internal, Humans, Steel, Treatment Outcome
Background
Fracture at the posterior malleolar is very common, accounting for about 14% to 44% of total ankle fractures [1,2]. When a posterior malleolus fracture with medial and lateral malleolus fracture occurs, the clinical prognosis of patients becomes significantly worse [3].
Haraguchi et al divided posterior malleolus fractures into 3 types according to the results of computed tomography (CT) scanning [4]. Type I is a posterolateral oblique fracture (67%), and most of this type contain triangular fracture blocks on the posterolateral side of the distal tibia. Type II is the medial extension type (19%), which extends from the fibular tubercle of the distal tibia to the medial malleolus. This type is mostly seen in trimalleolar fractures and often contains 2 parts of fracture blocks, namely the posteromedial fracture block and posterolateral fracture block. Type III is the small bone block type (14%), which is composed of one or more small bone blocks of the posterior lip of the tibia. Mason et al [5] divided posterior malleolar fractures into 3 types according to the results of CT scanning. Type I is an extraarticular avulsion fracture, which is caused by the traction of the posterior tibiofibular ligament. Type IIA is the posterolateral Volkmann fracture, in which the fracture line extends to the tibial fibular notch and is caused by the impact of the rotating talus when the ankle is in plantar flexion. Type IIB is a 2-part fracture of the posterior malleolus, namely a posterior medial fracture and posterior lateral fracture. After a posterior lateral fracture, when the talus continues to rotate in the ankle point, a posterior medial fracture can be caused. Type III involves the whole posterior ankle on the coronal plane, which is the posterior pilon fracture caused by axial violence. In this study, the fracture types included were 2-part fractures of the posterior malleolus, namely type II in Haraguchi classification and type IIB in Mason classification.
The anatomical characteristics of the posterior malleolus and their importance in stabilizing the ankle joint have received increasing attention by clinicians and have become the focus of recent clinical research. For common trimalleolar fractures, lateral and posterior malleolus fractures can be treated through the posterolateral approach, and the medial approach can be used to treat medial malleolus fractures. This treatment principle has been widely used. However, when medial and lateral malleolar fractures are combined with fractures of the posterior malleolar and the fracture line extends to the rear of the medial malleolus, the clinician cannot see the joint reduction under direct vision in surgery if the conventional anterior approach is used. However, if the posterior medial approach, which needs to avoid the posterior tibial vessels and nerves, is adopted, the risk and difficulty of surgery increases, and iatrogenic injury can be easily caused.
We present a technique of approaching this fracture pattern with direct reduction and fixation without extensive soft tissue dissection. This modified posterolateral approach has obvious advantages, such as a good surgical field, few important blood vessels and nerves involved in the surgery, and a fully exposed fracture site. Also, only 1 incision is needed to reduce the 2 fractures of lateral malleolus and posterior malleolus under direct vision. From January 2018 to January 2020, we treated 12 patients with medial and lateral malleolus fractures with posterior malleolus fractures in the floating position through a modified posterolateral approach. In addition, the exposure effect of posterior medial and lateral bone blocks and the reduction and fixation effect of medial and lateral malleolus fractures were evaluated.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria were as follows: 1) patients with acute ankle fracture; 2) patients with lateral malleolus fracture with oblique fracture line at the lower end of tibiofibular syndesmosis; and 3) patients with posterior malleolus fracture with 2 bone blocks at the inner and outer sides. The exclusion criteria were as follows: 1) patients with old ankle fracture; 2) patients with triangular ligament injury; and 3) patients who could not tolerate the surgery.
BASIC PATIENT INFORMATION:
A total of 12 patients were included in the study, including 5 men and 7 women, aged from 29 to 66 years (average, 49 years). The causes of injury were accidental falls and sprains when going down stairs or stepping on a low stool. The symptom was unilateral medial and lateral malleolus fracture with 2-part fracture of the posterior malleolus. The fracture lines of the lateral malleolus were long and oblique, located at the lower end of tibiofibular syndesmosis. Medial malleolus fractures were triangular ligament traction avulsion fractures without triangular ligament injury. The classification of posterior malleolus fractures was Haraguchi II, that is, the posterior malleolus fracture was divided into posterolateral and posteromedial fractures, involving the posterior fracture of medial malleolus. The symptoms of all patients were closed fracture, no combined injury, and no surgical contraindication. All patients underwent anteroposterior and lateral X-rays of the ankle joint and 3-dimensional reconstruction by CT scan before surgery. According to the fracture and swelling of the patients, calcaneal tubercle traction was selected for treatment, and surgery was performed 5 to 12 days (average, 10 days) after injury. All patients gave their written informed consent.
SURGICAL PROCEDURE:
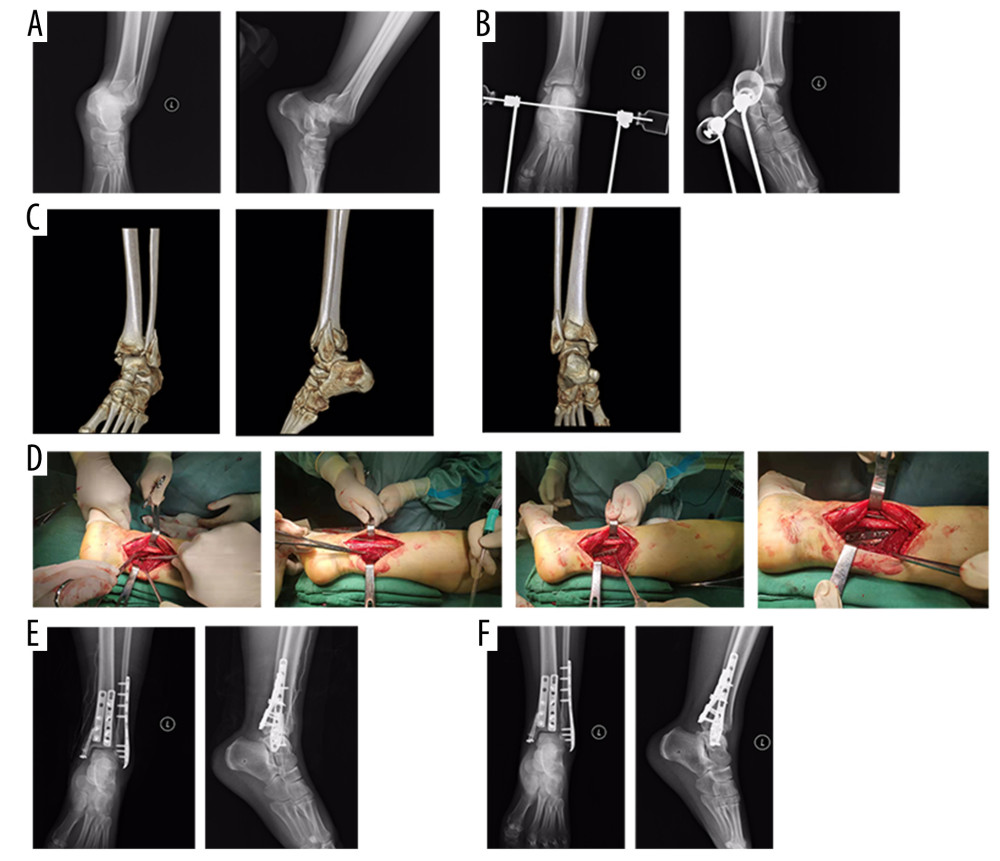
Surgery was performed under the floating position, using subarachnoid anesthesia or nerve block anesthesia and an air bag tourniquet. The combined posteromedial and posterolateral approach was used. The posterolateral approach was located 1 cm behind the fibula, with a total length of about 10 to 14 cm, and its distal end arced to the fibular tip. The surgeon entered between the peroneus longus, peroneus brevis, and the flexor hallucis longus tendon to expose the posterior malleolar and medial and external bone blocks. During the operation, attention was paid to protect the sural nerve. At the fracture of the lateral malleolus, the surgeon entered from the front of the peroneal tendon, showing 2 windows in 1 incision together with the above-mentioned approach. The muscle and soft tissue was then pushed along the posterior malleolar periosteum with the periosteal stripper, and the internal and external bone blocks of the posterior malleolar were fully exposed with the hip retractor. C-arm X-ray equipment was used for fluoroscopy of the anterior and lateral positions of ankle joint to clarify the reduction of fracture. Lateral steel plate fixation was performed for lateral malleolus fractures; the internal and external bone blocks of the posterior malleolus were fixed with 1 of 3 tubular steel plates of appropriate length, according to the size and displacement of bone blocks, and medial malleolus fractures were fixed with cannulated screws (Figure 1). After fixation, fluoroscopy was performed again to determine the appropriate position and length of the implant. Finally, the incision was closed layer by layer and negative pressure drainage was placed.
POSTOPERATIVE TREATMENT:
The affected limb was raised after surgery to disperse swelling. On the first day after surgery, passive flexion and extension exercises of the toe and ankle, straight leg lifting exercises of the quadriceps femoris, and flexion and extension exercises of the hip and knee joint were started. Active flexion and extension exercises of the toes and ankles were started on the second day after surgery, and walking with crutches was started according to the level of swelling. The sutures were removed 2 weeks after surgery. Weight-bearing walking was practiced 6 weeks after surgery, and the pain of the exercise was not to exceed the patient’s tolerance limit for pain. A medical imaging examination was performed at 1 month, 6 months, and 1 year after surgery, and the recovery of foot and ankle function was measured. At the last follow-up, the ankle hindfoot score and visual analog scale (VAS) of the American Orthopedic Foot and Ankle Society (AOFAS) [4] were used for evaluation.
STATISTICAL ANALYSIS:
IBM SPSS19.0 software was used for statistical analysis. The measurement data were tested by the Shapiro-Wilk test for normal distribution. The measurement data with normal distribution and homogeneous variance were represented by mean±standard deviation. The VAS scores before and after surgery were compared by the paired
Results
The average follow-up time of the 12 patients was 18 months (7–30 months). All patients had no infection, and their incisions healed in the first stage. Postoperative radiography showed that the average fracture healing time was 12.5 weeks (10–15 weeks). There were no patients with nonunion of fracture or loosening or fracture of internal fixation. The average time for the patients to walk weight bearing was 13 weeks (11–16 weeks), and none had obvious pain or discomfort. At the last follow-up, the average AOFAS ankle hindfoot score of the 12 patients was 87.5 (77–95), with 7 excellent and 5 good scores. The combined excellent and good rate was 100%. The VAS scores improved from before surgery (average 8.25 points) to after surgery (average 1 point), and the difference was statistically significant (
Discussion
The Lauge-Hansen classification of ankle fracture is based on the injury mechanism, not on CT results. It cannot explain the 2-part fracture of the posterior ankle. Mason et al believe that in the 2-part fracture of the posterior malleolus, when the ankle joint is in the plantar flexion position, the rotation of the talus in the ankle acupoint and impact of the posterior malleolus will first lead to the posterolateral fracture. When the stress continues to transfer inward, it will lead to the posteromedial bone at 45° to the posterolateral bone mass. There is still controversy regarding whether this type of fracture is a posterior ankle fracture or posterior pilon fracture. Previous studies showed that ankle fractures were caused by rotational violence and pilon fractures were caused by vertical violence. However, it has been found in clinical work that the causes of fracture in some patients include both rotational violence and vertical violence. The classification of fracture types should be based on which kind of violence is primary. In addition, it should be based on whether the fracture line of the posterior malleolus exceeds 50% of the tibial fibular notch or involves the anterior colliculus of the medial malleolus [6]. All patients in the present study group were subjected to vertical violence when they were injured (mostly when they went down the stairs). The vertical height was about 30 cm, and the vertical violence was relatively small. At this time, the toe hit the ground first, the ankle was in the plantar flexion position, and the talus was hit by rotational violence at the same time, resulting in the fracture of the lateral ankle, the posterior ankle, and the medial ankle at the same time. Therefore, the patients in this group were mainly subjected to rotational violence, supplemented by vertical violence. Switaj et al [7] proposed the concept of a posterior pilon-like variant ankle fracture. Of the 270 patients with ankle diseases they studied, 50% of patients had accompanied posterior malleolar fracture, of which 20% had a posterior pilon-like variant. The ankle fracture in their group of patients was caused by the simultaneous action of rotational violence and vertical violence, in which rotational violence played an important role. When the ankle joint was in the plantar flexion position, the rotation of the talus in the ankle point struck the posterior malleolus, resulting in an ankle fracture similar to the posterior pilon variant.
The surgical indications of posterior malleolar fractures have been recognized by researchers. Fixation of the posterior malleolus is conducive to the recovery of the articular surface, maintenance of fibula length, and stability of the lower tibiofibular end. It can also prevent the placement of screws in the lower tibiofibular, thereby achieving early functional exercise [8–11]. The classic posterolateral approach has been widely used in clinical settings. It is located in the middle of the posterior edge of fibula and the outer edge of Achilles tendon and enters between the fibular tendon and flexor longus tendon, which can expose the fracture of the lateral malleolus and Volkmann bone mass of the posterior malleolus at the same time [12]. Some authors have proposed a posteromedial approach between the flexor longus tendon and neurovascular bundle, which can fully expose the whole posterior ankle [13,14]. The posterolateral bone mass of the posterior malleolus can be accessed between the flexor longus tendon and the tibial nerve, while the posterior medial bone mass of the posterior malleolus can be accessed between the flexor digitorum longus tendon and the posterior tibial tendon. The incision lifts the whole posterior medial flap, resulting in a high risk of injury and infection in skin and soft tissue. The treatment method is to treat the posterior internal and external bone mass of the posterior ankle through different approaches in the ankle canal tissue, which needs to open the ankle canal and has the risk of causing irritation to the blood vessels, nerves, and tendons in the ankle canal. Based on the above, we used the modified posterolateral approach in the floating position to treat the patients in the present study. The posterolateral approach can fully expose the lateral malleolus fracture and the medial and lateral fracture blocks of the posterior malleolus, while the distal arc to the medial malleolus can expose the medial malleolus fracture.
Many surgical approaches to the posterior tibial plafond have been described. In the 2004 case series by Weber, 10 patients were treated with a posteromedial and posterolateral approach and at the 1-year follow-up, all were doing well clinically and radiographically [15]. In 2006, Bhattacharyya et al reported a posterolateral approach to pilon fractures in 19 patients, 6 of whom developed wound complications [16]. Kao described a “postero-medio-anterior” approach to pilon fractures that used a larger “J”-type incision that started posteriorly proximally and then curved around the medial malleolus and distally was located over the dorsomedial foot. There were no nerve injuries and there were 2 cases of superficial wound edge necrosis [17]. In the present study, there were no infections, wound healing problems, or nerve injuries, and the clinical results were acceptable.
The 2-part fracture of posterior malleolus complicated with medial and lateral malleolar fractures is one of the thorny problems faced by clinicians. This kind of fracture is caused by rotational violence and vertical violence at the same time. After injury, the ankle tends toward subluxation, so both bone and soft tissue may be injured. Traction of the calcaneal tubercle is conducive to detumescence, analgesia, and initial reduction and lays a good foundation for intraoperative anatomical reduction. The surgery is carried out in the floating position. The posterolateral incision can expose 2 related surgical windows, which is conducive to the anatomical reduction of posterior ankle fracture blocks, especially those with coronal rotation displacement. In conclusion, the 2-part fracture of the posterior malleolar complicated with medial and lateral malleolar fractures creates difficulty in clinical treatment. The modified posterolateral approach under the floating position can fully expose the fractures of the medial, lateral, and posterior malleolus at the same time, and thus carry out satisfactory reduction and reliable internal fixation. The advantage of this method is a good clinical effect, but the disadvantage is that exposing the posterior medial bone block from the posterolateral incision requires excessive traction of the soft tissue, which can cause soft tissue damage.
The limitations of this retrospective study are the small sample size and lack of comparative studies of different approaches. The effectiveness of this method can be evaluated through anatomical and biomechanical studies in the future. A large prospective randomized controlled study is expected to be carried out on patients with different surgical approaches to better guide the selection of treatment options and risk assessment.
Conclusions
The posterolateral approach through 1 incision, 2 windows, and 3 steel plates is effective in the treatment of 2-part posterior malleolus fractures complicated with medial and lateral malleolus fractures.
References
1. Koval KJ, Lurie J, Zhou W, Ankle fractures in the elderly: What you get depends on where you live and who you see: J Orthop Trauma, 2005; 19(9); 635-39
2. Bartoníček J, Rammelt S, Tuček M, Posterior malleolar fractures: changing concepts and recent developments: Foot Ankle Clin, 2017; 22(1); 125-45
3. Mingo-Robinet J, Abril Larrainzar JM, Valle Cruz JA, Posterolateral approach in trimalleolar ankle fractures: Surgical technique: Rev Esp Cir Ortop Traumatol, 2012; 56(4); 313-18
4. Haraguchi N, Haruyama H, Toga H, Pathoanatomy of posterior malleolar fractures of the ankle: J Bone Joint Surg Am, 2006; 88; 1085-92
5. Mason LW, Marlow WJ, Widnall J, Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle: Foot Ankle Int, 2017; 38(11); 1229-35
6. Bartoníček J, Rammelt S, Tuček M, Posterior malleolar fractures: changing concepts and recent developments: Foot Ankle Clin, 2017; 22(1); 125-45
7. Switaj PJ, Weatherford B, Fuchs D, Evaluation of posterior malleolar fractures and the posterior pilon variant in operatively treated ankle fractures: Foot Ankle Int, 2014; 35(9); 886-95
8. Gonzalez TA, Watkins C, Drummond R, Transfibular approach to posterior malleolus fracture fixation: Technique tip: Foot Ankle Int, 2016; 37(4); 440-45
9. Abdelgawad AA, Kadous A, Kanlic E, Posterolateral approach for treatment of posterior malleolus fracture of the ankle: J Foot Ankle Surg, 2011; 50(5); 607-11
10. Karachalios T, Roidis N, Karoutis D, Trimalleolar fracture with a double fragment of the posterior malleolus: A case report and modified operative approach to internal fixation: Foot Ankle Int, 2001; 22(2); 144-49
11. Solan MC, Sakellariou A, Posterior malleolus fractures: worth fixing: Bone Joint J, 2017; 99-B(11); 1413-19
12. Abdelgawad AA, Kadous A, Kanlic E, Posterolateral approach for treatment of posterior malleolus fracture of the ankle: J Foot Ankle Surg, 2011; 50(5); 607-11
13. Hoekstra H, Rosseels W, Rammelt S, Direct fixation of fractures of the posterior pilon via a posteromedial approach: Injury, 2017; 48(6); 1269-74
14. Wang Y, Wang J, Luo CF, Modified posteromedial approach for treatment of posterior pilon variant fracture: BMC Musculoskelet Disord, 2016; 17; 328
15. Weber M, Trimalleolar fractures with impaction of the posteromedial tibial plafond: Implications for talar stability: Foot Ankle Int, 2004; 25; 716-27
16. Bhattacharyya T, Crichlow R, Gobezie R, Complications associated with the posterolateral approach for pilon fractures: J Orthop Trauma, 2006; 20; 104-7
17. Kao KF, Huang PJ, Chen YW, Postero-medio-anterior approach of the ankle for the pilon fracture: Injury, 2000; 31; 71-74
In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952