01 April 2022: Clinical Research
A Retrospective Study of 881 Lateral Transabdominal Laparoscopic Adrenalectomies Performed Between 1997 and 2017 at a Single Center in Poland to Determine Factors Associated with Surgery Time
Milena Duralska1ABCDEF*, Jacek Dzwonkowski1ABDE, Janusz SierdzińskiDOI: 10.12659/MSM.936272
Med Sci Monit 2022; 28:e936272
Abstract
BACKGROUND: Laparoscopic adrenalectomy is acknowledged as a standard procedure in adrenal lesions management. This retrospective study of lateral transabdominal laparoscopic adrenalectomy performed between 1997 and 2017 in a single center in Poland aimed to determine the factors associated with surgery time.
MATERIAL AND METHODS: This retrospective study involved 881 patients. The factors identified as potentially affecting surgery time were age, sex, side of the lesion, histopathological type, hormonal activity, size of the lesion, history of previous abdominal operations, presence of intra-abdominal adhesions, and obesity. The following statistical tests were conducted: t test, Mann-Whitney U test, Kruskal-Wallis H test, Pearson correlation test, and multivariate regression modeling.
RESULTS: The mean surgery time for all operations was 139 min (55-320 min). We observed statistically significant differences for surgery time in the following groups: sex, side of the lesion, presence of intra-abdominal adhesions, obesity, histopathological type, and hormonal activity (P<0.05). The multivariate regression model showed factors affecting surgery time were: sex, side of the lesion, size of the lesion, obesity, histopathological type (nodular hyperplasia and adenoma), and hormonal activity (non-functioning and aldosterone-secreting tumors) (P<0.05). There was no correlation between surgery time and patient age and tumor size (P<0.05). Mean tumor size was 42 mm (6-130 mm).
CONCLUSIONS: The 20-year experience of laparoscopic adrenalectomy performed at a single center showed that surgery duration was significantly longer in male patients, obese patients, left-sided adrenal tumors, tumors >6 cm in diameter, patients with a diagnosis of pheochromocytoma, and when intra-abdominal adhesions were present.
Keywords: Adrenal Gland Neoplasms, Adrenalectomy, Laparoscopy, operative time, Humans, Male, Poland
Background
Laparoscopic adrenalectomy is acknowledged as a standard procedure in management of adrenal lesions. The operation was first performed by Gagner in 1992 [1]. Compared to the open method, it is associated with better outcomes and reduction in morbidity, less postoperative pain, shorter length of hospital stay, lower complications rate, and less operative blood loss, as well as less hemodynamic instability in pheochromocytoma, faster recovery, and better cosmetic results [2–8]. Several methods of endoscopic adrenalectomy have been described: lateral transabdominal, posterior or lateral retroperitoneoscopic, and lateral robotic [7,8]. The most popular are lateral transabdominal and posterior retroperitoneoscopic approaches [7,8]. It is recommended that surgeons use the technique most familiar to them to reach maximal safety and effectiveness [7,8].
The surgery time of laparoscopic adrenalectomy can be influenced by various factors; the most widely discussed in the literature are the size of the lesion, histopathological type, and surgeon’s experience [8–27]. The other important aspect is the volume of the center [8]. The European Society of Endocrine Surgeons published a consensus statement recommending that adrenal surgery should be performed only in centers performing at least 6 adrenalectomies per year [8]. The biggest series of patients operated on in a single institution and reported in the literature are 653 laparoscopic adrenalectomies over 24 years in the United States, 520 laparoscopic adrenalectomies over 20 years in France, 560 retroperitoneoscopic adrenalectomies over 12 years in Germany, and 245 laparoscopic adrenalectomies over 4 years in Poland [9–12].
Knowing the factors responsible for prolonged surgery can be useful in predicting difficult laparoscopic adrenalectomy. Therefore, this retrospective study from a single center in Poland included 881 patients who underwent lateral transabdominal laparoscopic adrenalectomy between 1997 and 2017 and aimed to determine the factors associated with surgery time.
Material and Methods
STUDY POPULATION AND STUDY DESIGN:
The study was approved by the Bioethics Committee at the Medical University of Warsaw (approval no. AKBE/65/2019).
We conducted a retrospective study of the 991 laparoscopic adrenalectomies performed in the Department of General, Vascular and Transplant Surgery, Medical University of Warsaw from 1997 to 2017. This is a high-volume tertiary referral center. All operations were performed by 1 experienced surgeon, Prof. Maciej Otto, and his team specializing in endocrine and laparoscopic surgery.
Exclusion criteria were: additional procedures performed together with adrenalectomy (cholecystectomy, hernia repair), bilateral adrenalectomy, conversion to open surgery, and adrenal-sparing procedure. The first 30 surgeries were included into the learning curve and were excluded from the analysis. Data of patients undergoing adrenalectomy from the open approach were not analyzed in this study.
DATA COLLECTION AND ANALYZED PARAMETERS:
The factors identified as potentially affecting surgery time were age, sex, side of the lesion, histopathological type, hormonal activity, size of the lesion, history of previous abdominal operations, presence of intra-abdominal adhesions, and obesity. Surgery time was counted from skin incision to skin closure. Histopathological results were divided into 5 groups: pheochromocytoma, adenoma, nodular hyperplasia, adrenocortical cancer and metastasis, and a group of other rarely occurring lesions. The hormonal activity was categorized as: lesions secreting glucocorticoids, lesions secreting mineralocorticoids, lesions secreting catecholamines, lesions secreting androgens, and hormonally inactive. The tumor size criterion used in our analysis was based on postoperative measurement performed by the pathologist during the histopathological examination. The previous abdominal operations category was split into 3 groups: no previous abdominal operations, 1 previous abdominal operation, and 2 and more previous abdominal operations. Intra-abdominal adhesions were defined as presence of strong adhesions requiring blunt and/or sharp dissection in the surgical area.
PERIOPERATIVE PROCEDURAL DETAILS:
All patients underwent pre-operative endocrinological workup, including imaging and hormonal studies, as well as pharmacological preparation when needed. Prior to surgery, all patients signed a written patients’ informed consent form for the operation. The lateral transabdominal approach was used as the surgical method of choice in all cases. The surgical method was previously described in the literature by the operating surgeon and our team [28,29].
STATISTICAL ANALYSIS:
All data were collected and saved in an electronic spreadsheet (Microsoft Excel). Statistical analysis was performed using the SAS 9.4 program. In addition to standard descriptive statistics, we conducted a
Results
DEMOGRAPHICS AND CLINICAL PATIENTS’ CHARACTERISTICS:
Data of 991 laparoscopic adrenalectomies were analyzed. After applying exclusion criteria, 110 operations were eliminated from statistical analysis (Table 1). A total of 881 operations were evaluated. Patient demographics are summarized in Table 2. There were 606 females and 275 males. Mean age was 53.6 years and standard deviation (SD) was 13.9 years. There were 397 left-sided tumors and 484 right-sided tumors. Histopathological diagnoses included pheochromocytomas (n=178), adenomas (n=391), nodular hyperplasia (n=177), malignancies (n=27 [9 adrenocortical cancer and 18 metastasis]), and other tumors (n=108). The group of other tumors is characterized in Table 3. Hormonal activity diagnoses included non-functioning lesions (n=410), aldosterone-secreting tumors (n=92), cortisol-secreting tumors (n=187), catecholamines-secreting tumors (n=179), and androgens-secreting tumors (n=13). Mean tumor size was 42 mm (6–130 mm), median=40 mm, SD=20 mm. There were 304 patients who underwent 1 abdominal operation prior to laparoscopic adrenalectomy and 89 patients who underwent at least 2 abdominal operations prior to laparoscopic adrenalectomy. Intra-abdominal adhesions were present in 204 operations and obesity in 202 patients.
VARIABLES ASSOCIATED WITH THE RISK OF PROLONGED SURGERY TIME:
Mean surgery time for all operations was 139 min (55–320 min), median=130 min, SD=42 min. Descriptive statistics for surgery time in particular groups are shown in Table 2. We observed statistically significant differences for surgery time in the following groups: sex, side of the lesion, presence of intra-abdominal adhesions, and obesity (P<0.05). Duration of surgery was longer in male patients, left-sided adrenal tumors, obese patients, and when intra-abdominal adhesions were present.
When comparing the surgery time in histopathological groups, we found statistically significant differences for pheochromocytoma, adenoma, and the group of other tumors (chi-square=24.17, P=0.0001). Pheochromocytoma resection was the longest procedure, while adenoma resection was the shortest procedure (Figure 1). In hormonal activity comparison, there were statistically significant differences in surgery time for all groups apart from androgens-secreting tumors (chi-square=27.84, P=0.0001). Resection of catecholamines-secreting tumors was the longest operation and resection of aldosterone-secreting tumors was the shortest operation (Figure 2). There were no statistically significant differences in surgery time in groups of patients who underwent previous operations (P=0.14) (Figure 3).
The multivariate regression model (F=31.06, P<0.0001) showed that the following factors were associated with surgery time: sex, side of the lesion, size of the lesion, obesity, histopathological type (nodular hyperplasia and adenoma), and hormonal activity (non-functioning and aldosterone-secreting tumors). The model confirmed that surgery time was longer in male patients, left-sided adrenal tumors, lesion size above 6 cm, and in obese patients. Surgery time was shorter in nodular hyperplasia lesions and adenoma, as well as non-functioning and aldosterone-secreting tumors (Table 4). Age, history of previous abdominal operations, and presence of intra-abdominal adhesions were not significantly associated with surgery time in the multivariate regression model.
There was no correlation between surgery time and patient age (correlation coefficient (r)=0.01;
Discussion
STUDY LIMITATIONS:
We would also like to address some limitations of our study. Its retrospective character did not allow us to evaluate some factors which could be associated with surgery time due to lack of data in medical documentation. We could only isolate information regarding obesity, but not exact BMI. Periadrenal fat volume is another possibly significant factor that we could not evaluate. The last factor is the type of dissecting instrument used, as technology was improving and equipment was changing over time. The study would also have benefited from separately assessing the durations of specific parts of the operation, such as exposing the adrenal loggia, tumor dissection, and identification of the adrenal vein.
Conclusions
The 20-year experience of laparoscopic adrenalectomy performed at a single center showed that surgery time was significantly longer in male patients, obese patients, left-sided adrenal tumors, tumors >6 cm in diameter, patients with a diagnosis of pheochromocytoma, and when intra-abdominal adhesions were present.
Figures
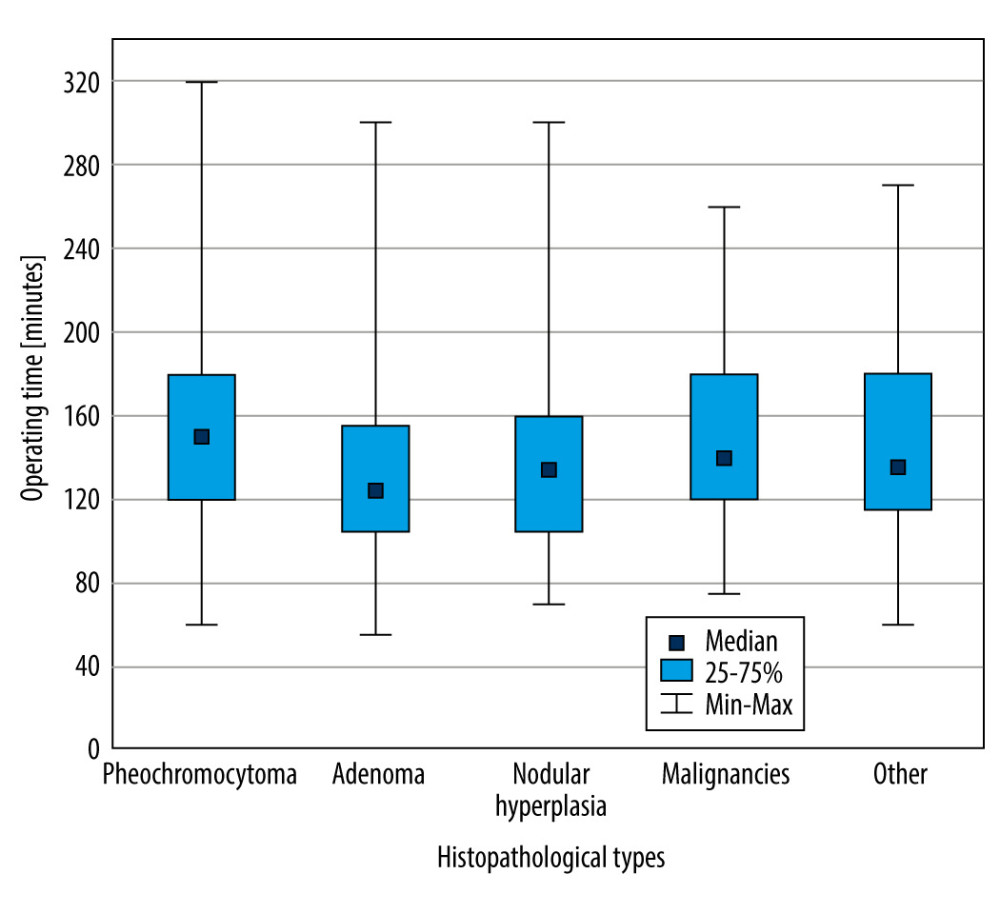 Figure 1. Box and whisker plot of surgery time in various histopathological types (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 1. Box and whisker plot of surgery time in various histopathological types (Kruskal-Wallis H test) (Microsoft Office 2019). 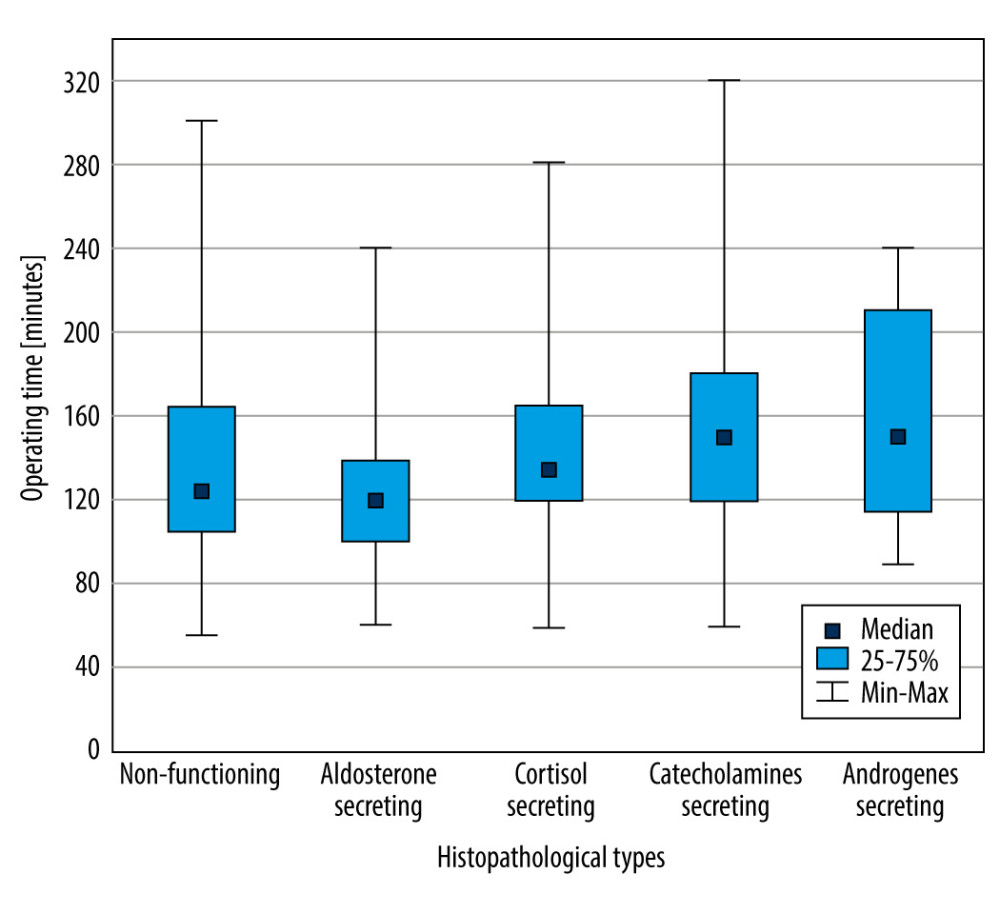 Figure 2. Box and whisker plot of surgery time in various hormonal activity groups (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 2. Box and whisker plot of surgery time in various hormonal activity groups (Kruskal-Wallis H test) (Microsoft Office 2019). 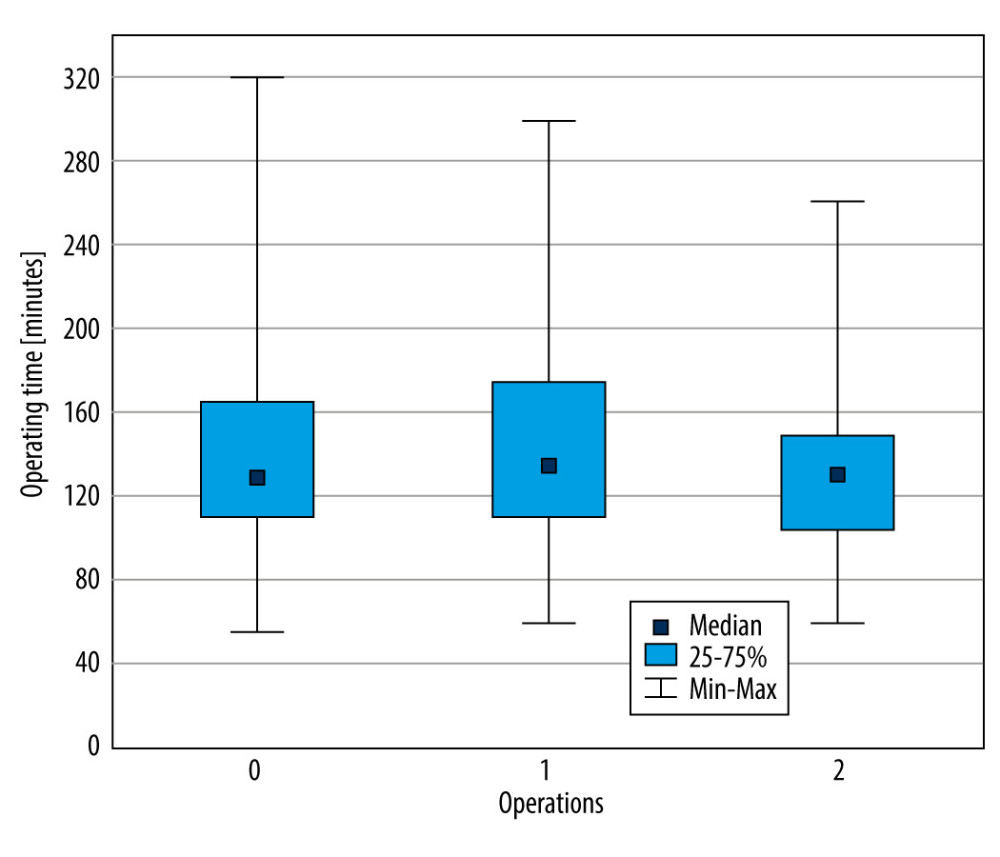 Figure 3. Box and whisker plot of surgery time in the number of previous operations (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 3. Box and whisker plot of surgery time in the number of previous operations (Kruskal-Wallis H test) (Microsoft Office 2019). References
1. Gagner M, Lacroix A, Bolté E, Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma: N Engl J Med, 1992; 327(14); 1033
2. Hazzan D, Shiloni E, Golijanin D, Jurim O, Laparoscopic vs open adrenalectomy for benign adrenal neoplasm: Surg Endosc, 2001; 15(11); 1356-58
3. Bai S, Yao Z, Zhu X, Comparison of transperitoneal laparoscopic versus open adrenalectomy for large pheochromocytoma: A retrospective propensity score-matched cohort study: Int J Surg, 2019; 61; 26-32
4. Zhu W, Wang S, Du G, Comparison of retroperitoneal laparoscopic versus open adrenalectomy for large pheochromocytoma: A single-center retrospective study: World J Surg Oncol, 2019; 17(1); 111
5. Elfenbein DM, Scarborough JE, Speicher PJ, Scheri RP, Comparison of laparoscopic versus open adrenalectomy: results from American College of Surgeons-National Surgery Quality Improvement Project: J Surg Res, 2013; 184(1); 216-20
6. Lubikowski J, Umiński M, Andrysiak-Mamos E, From open to laparoscopic adrenalectomy: Thirty years’ experience of one medical centre: Endokrynol Pol, 2010; 61(1); 94-101
7. Stefanidis D, Goldfarb M, Kercher KW, SAGES guidelines for minimally invasive treatment of adrenal pathology: Surg Endosc, 2013; 27(11); 3960-80
8. Mihai R, Donatini G, Vidal O, Brunaud L, Volume-outcome correlation in adrenal surgery-an ESES consensus statement: Langenbecks Arch Surg, 2019; 404(7); 795-806
9. Chen Y, Scholten A, Chomsky-Higgins K, Risk factors associated with perioperative complications and prolonged length of stay after laparoscopic adrenalectomy: JAMA Surg, 2018; 153(11); 1036-41
10. Coste T, Caiazzo R, Torres F, Laparoscopic adrenalectomy by transabdominal lateral approach: 20 years of experience [published correction appears in Surg Endosc 2017;31(7): 2752]: Surg Endosc, 2017; 31(7); 2743-51
11. Walz MK, Alesina PF, Wenger FA, Posterior retroperitoneoscopic adrenalectomy – results of 560 procedures in 520 patients: Surgery, 2006; 140(6); 943-50
12. Pogorzelski R, Toutounchi S, Krajewska E, The usefulness of laparoscopic adrenalectomy in the treatment of adrenal neoplasms – a single-centre experience: Endokrynol Pol, 2017; 68(4); 407-10
13. Conzo G, Gambardella C, Candela G, Single center experience with laparoscopic adrenalectomy on a large clinical series: BMC Surg, 2018; 18(1); 2
14. Battistella E, Ferrari S, Pomba L, Toniato A, Adrenal surgery: Review of 35 years experience in a single centre: Surg Oncol, 2021; 37; 101554
15. Di Buono G, Buscemi S, Lo Monte AI, Laparoscopic adrenalectomy: Preoperative data, surgical technique and clinical outcomes: BMC Surg, 2019; 18(Suppl 1); 128
16. Natkaniec M, Dworak J, Pędziwiatr M, Patients criteria determining difficulty of the laparoscopic lateral transperitoneal adrenalectomy. A retrospective cohort study: Int J Surg, 2017; 43; 33-37
17. Castillo OA, Vitagliano G, Secin FP, Laparoscopic adrenalectomy for adrenal masses: Does size matter?: Urology, 2008; 71(6); 1138-41
18. Gumbs AA, Gagner M, Laparoscopic adrenalectomy: Best Pract Res Clin Endocrinol Metab, 2006; 20(3); 483-99
19. Asari R, Koperek O, Niederle B, Endoscopic adrenalectomy in large adrenal tumors: Surgery, 2012; 152(1); 41-49
20. Kalady MF, McKinlay R, Olson JA, Laparoscopic adrenalectomy for pheochromocytoma. A comparison to aldosteronoma and incidentaloma: Surg Endosc, 2004; 18(4); 621-25
21. Alesina PF, Walz MK, Adrenal tumors: Are gender aspects relevant?: Visc Med, 2020; 36(1); 15-19
22. Tiberio GA, Solaini L, Arru L, Factors influencing outcomes in laparoscopic adrenal surgery: Langenbecks Arch Surg, 2013; 398(5); 735-43
23. Natkaniec M, Pędziwiatr M, Wierdak M, Laparoscopic adrenalectomy for pheochromocytoma is more difficult compared to other adrenal tumors: Wideochir Inne Tech Maloinwazyjne, 2015; 10(3); 466-71
24. Fassnacht M, Arlt W, Bancos I, Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors: Eur J Endocrinol, 2016; 175(2); G1-34
25. Boylu U, Oommen M, Lee BR, Thomas R, Laparoscopic adrenalectomy for large adrenal masses: Pushing the envelope: J Endourol, 2009; 23(6); 971-75
26. Parnaby CN, Chong PS, Chisholm L, The role of laparoscopic adrenalectomy for adrenal tumours of 6 cm or greater: Surg Endosc, 2008; 22(3); 617-21
27. Conzo G, Tartaglia E, Gambardella C, Minimally invasive approach for adrenal lesions: Systematic review of laparoscopic versus retroperitoneoscopic adrenalectomy and assessment of risk factors for complications: Int J Surg, 2016; 28(Suppl 1); S118-23
28. Otto M, Szostek G, Nazarewski S, Laparoscopic operative technique for adrenal tumors: JSLS, 2000; 4(2); 125-29
29. Otto M, Dzwonkowski J, Jędrasik M, Qualification and operative difficulties of laparoscopic adrenalectomy: Polish Journal of Surgery, 2010; 82(1); 38-46
30. Goitein D, Mintz Y, Gross D, Reissman P, Laparoscopic adrenalectomy: Ascending the learning curve [published correction appears in Surg Endosc. 2004;18(10): 1542]: Surg Endosc, 2004; 18(5); 771-73
31. Alberici L, Ricci C, Ingaldi C, The learning curve for the second generation of laparoscopic surgeons: Lesson learned from a large series of laparoscopic adrenalectomies: Surg Endosc, 2021; 35(6); 2914-20
32. Pearlstein SS, Kuo JH, Chabot JA, Lee JA, Periadrenal volume is a better predictor of prolonged operative time in laparoscopic retroperitoneal adrenalectomy than BMI: World J Surg, 2020; 44(2); 578-84
33. Toutounchi S, Pogorzelski R, Legocka ME, Lateral laparoscopic adrenalectomy in patients with previous abdominal surgery – single-center experience: Wideochir Inne Tech Maloinwazyjne, 2018; 13(3); 283-87
34. Pędziwiatr M, Matłok M, Kulawik J, Laparoscopic adrenalectomy by the lateral transperitoneal approach in patients with a history of previous abdominal surgery: Wideochir Inne Tech Maloinwazyjne, 2013; 8(2); 146-51
35. Kazaryan AM, Marangos IP, Røsok BI, Impact of body mass index on outcomes of laparoscopic adrenal surgery: Surg Innov, 2011; 18(4); 358-67
36. Inaishi T, Kikumori T, Takeuchi D, Obesity does not affect peri- and postoperative outcomes of transabdominal laparoscopic adrenalectomy: Nagoya J Med Sci, 2018; 80(1); 21-28
Figures
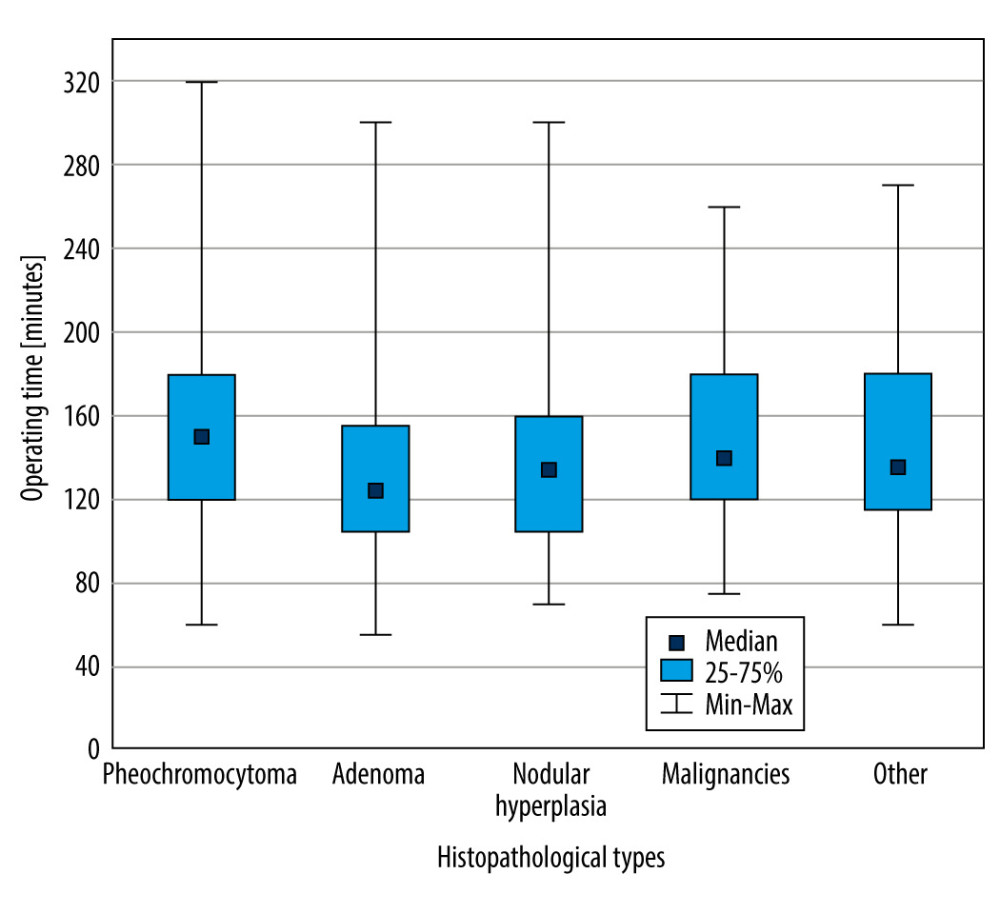 Figure 1. Box and whisker plot of surgery time in various histopathological types (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 1. Box and whisker plot of surgery time in various histopathological types (Kruskal-Wallis H test) (Microsoft Office 2019).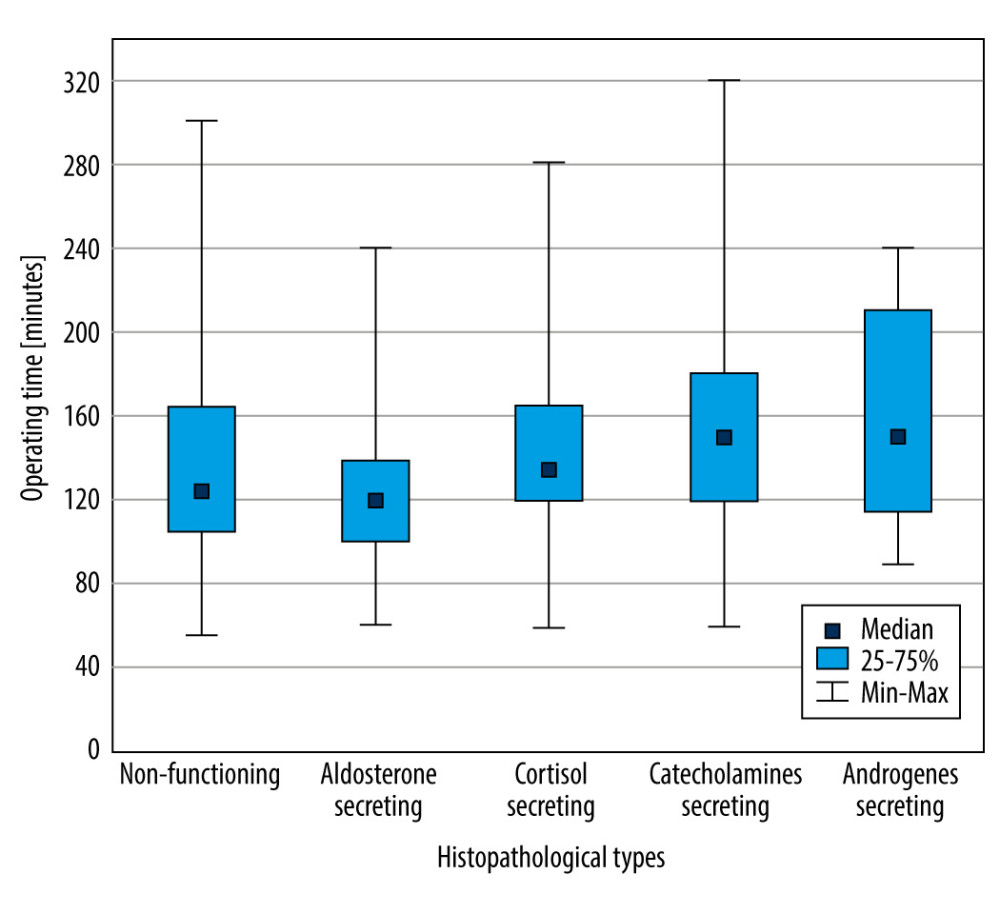 Figure 2. Box and whisker plot of surgery time in various hormonal activity groups (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 2. Box and whisker plot of surgery time in various hormonal activity groups (Kruskal-Wallis H test) (Microsoft Office 2019).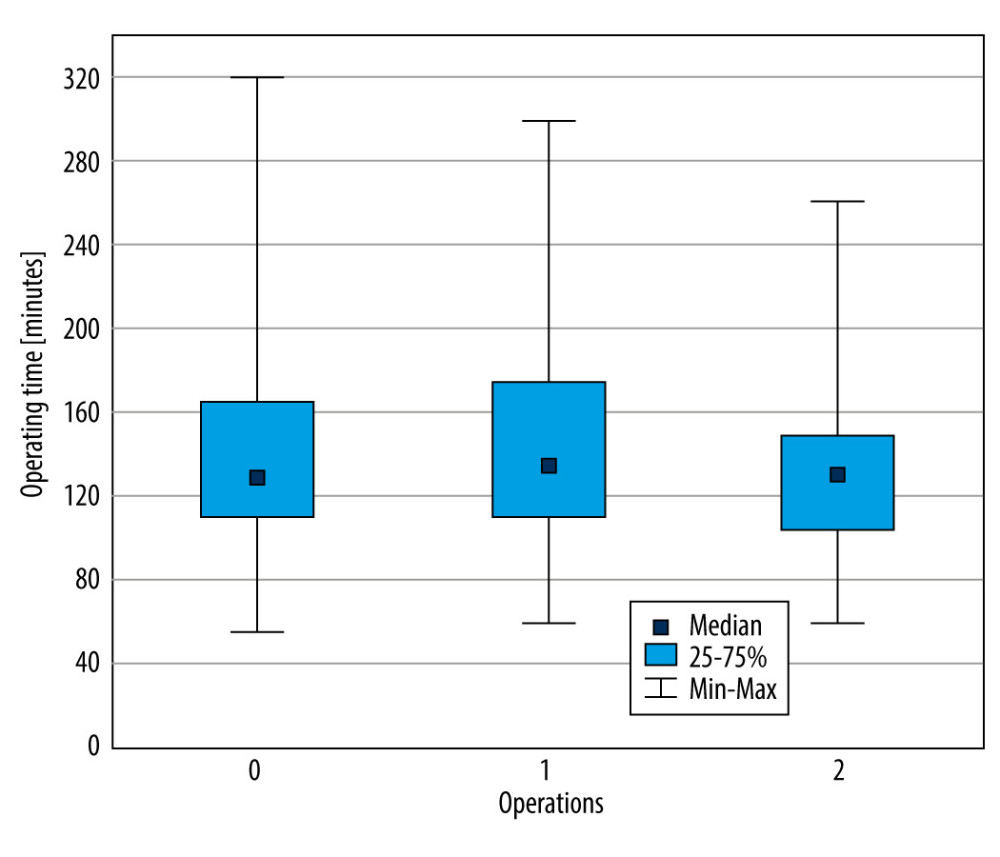 Figure 3. Box and whisker plot of surgery time in the number of previous operations (Kruskal-Wallis H test) (Microsoft Office 2019).
Figure 3. Box and whisker plot of surgery time in the number of previous operations (Kruskal-Wallis H test) (Microsoft Office 2019). Tables
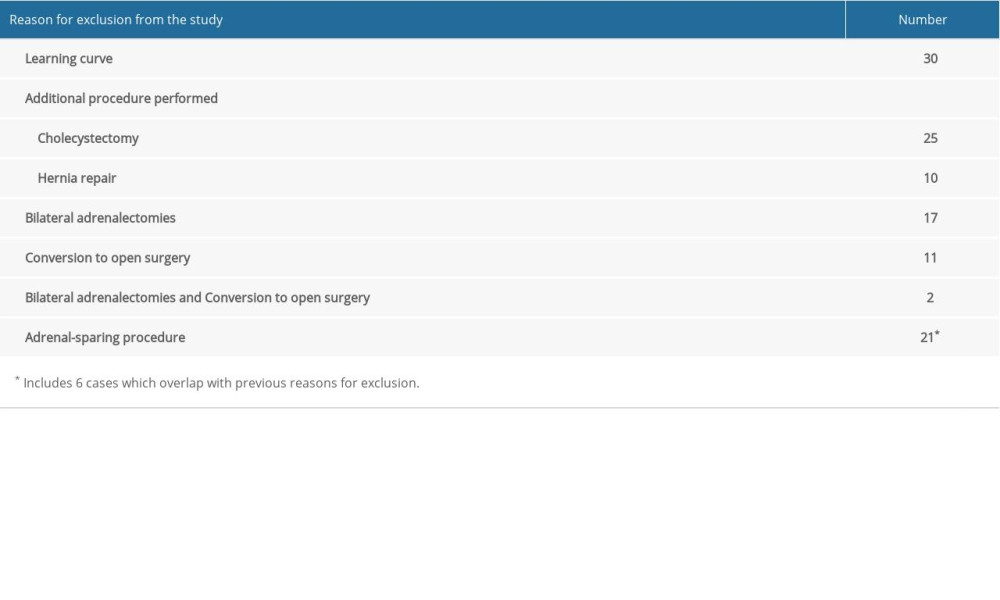 Table 1. Reasons for exclusion from the study.
Table 1. Reasons for exclusion from the study.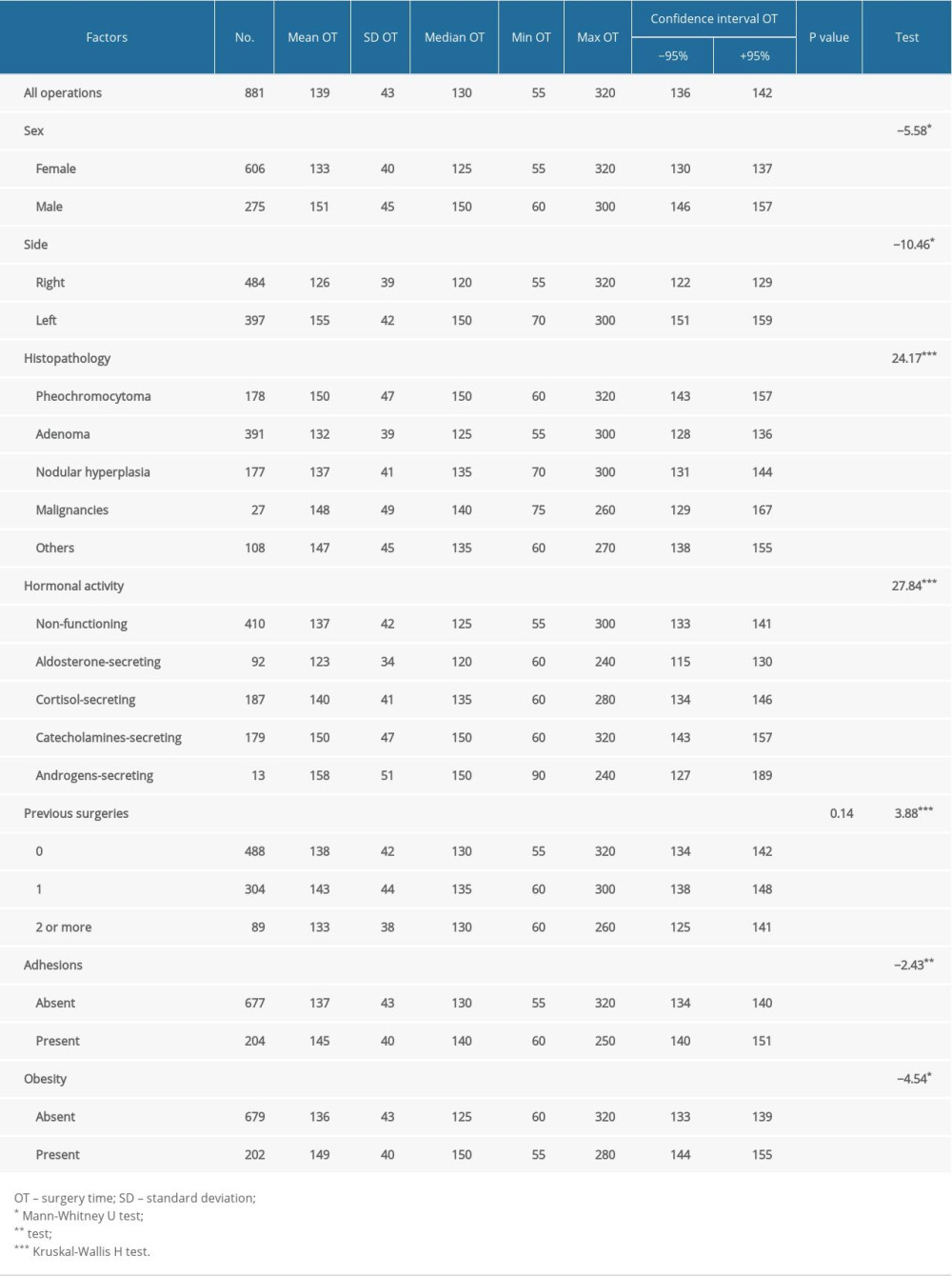 Table 2. Patient demographics and statistical analysis of surgery time.
Table 2. Patient demographics and statistical analysis of surgery time. Table 3. Characteristic of the group of other tumors.s
Table 3. Characteristic of the group of other tumors.s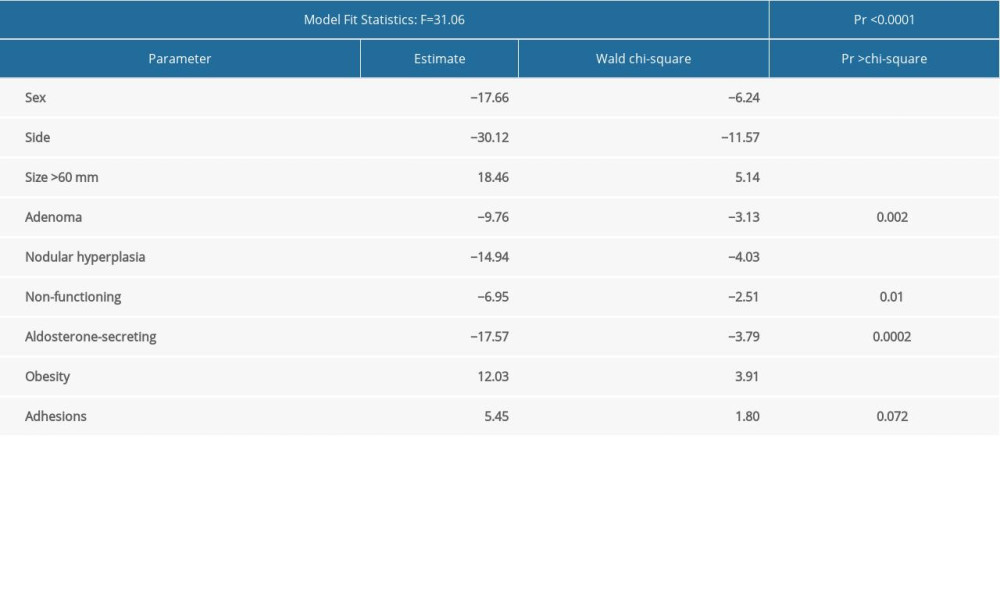 Table 4. Multivariate regression model on surgery time (F Value 31.06).
Table 4. Multivariate regression model on surgery time (F Value 31.06).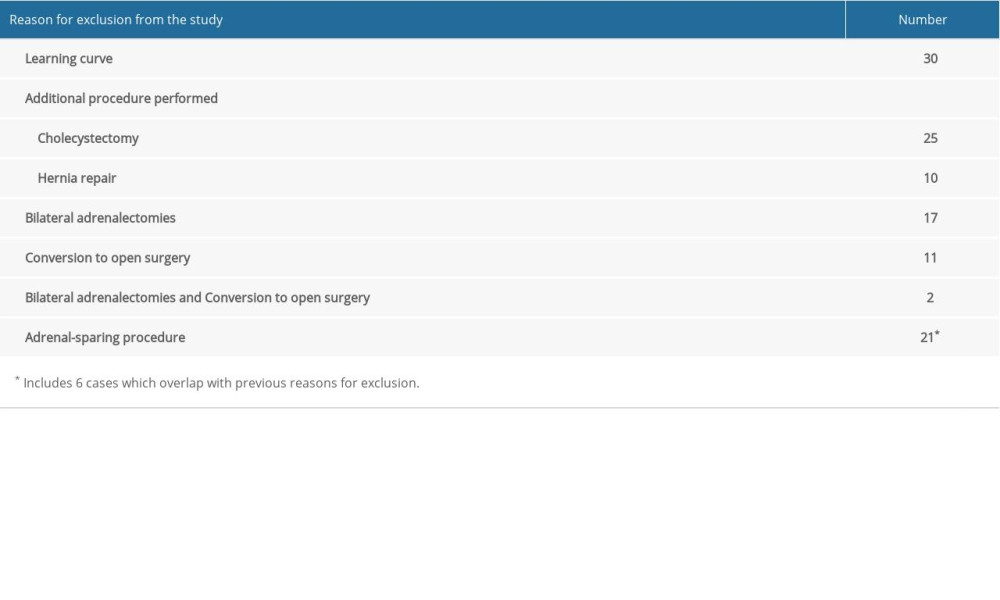 Table 1. Reasons for exclusion from the study.
Table 1. Reasons for exclusion from the study.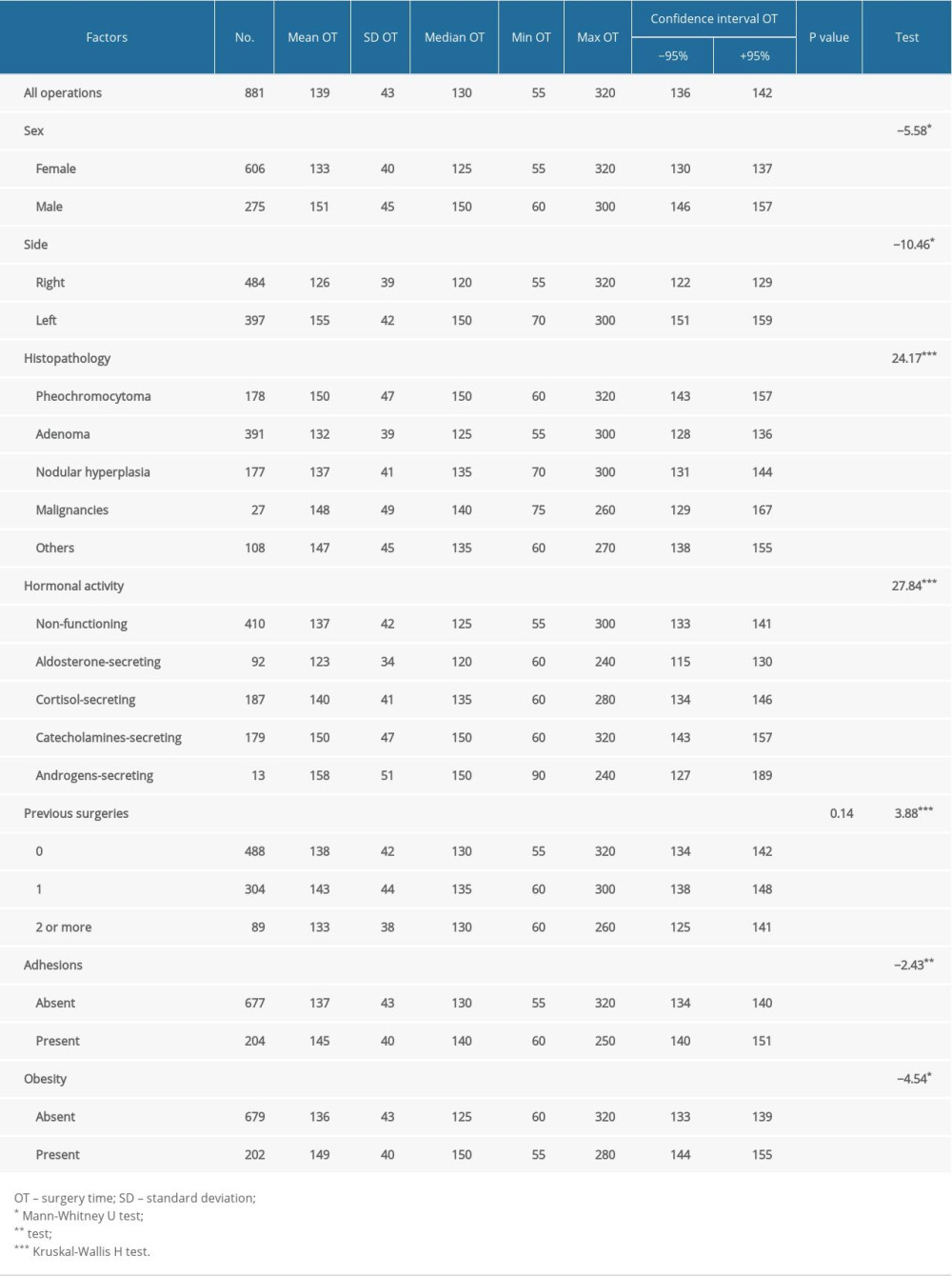 Table 2. Patient demographics and statistical analysis of surgery time.
Table 2. Patient demographics and statistical analysis of surgery time. Table 3. Characteristic of the group of other tumors.s
Table 3. Characteristic of the group of other tumors.s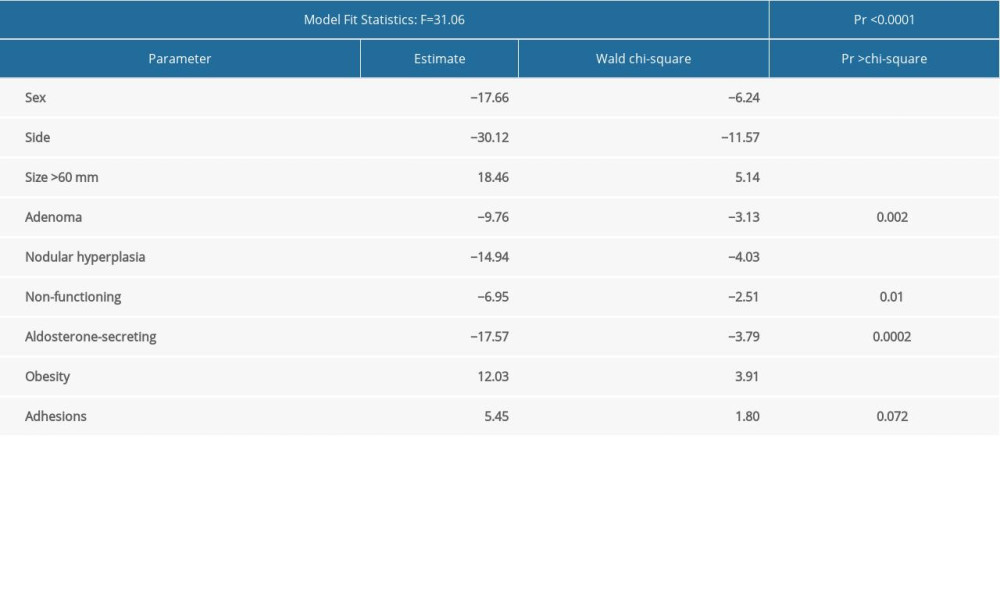 Table 4. Multivariate regression model on surgery time (F Value 31.06).
Table 4. Multivariate regression model on surgery time (F Value 31.06). In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








