23 April 2024: Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debridement with and without Methylene Blue Injection
Zheng ZhouDOI: 10.12659/MSM.941102
Med Sci Monit 2024; 30:e941102
Abstract
BACKGROUND: This retrospective study of 42 patients with popliteal cysts (or Baker cysts) aimed to compare the effects on duration and outcomes of arthroscopic surgical debridement with and without the use of cyst injection with methylene blue (MB).
MATERIAL AND METHODS: Medical records of patients who underwent conventional arthroscopic surgery (n=20) or arthroscopic surgery after MB injection (n=22) for popliteal cysts between 2018 and 2021 were reviewed. The MB group underwent arthroscopic popliteal cystectomy with MB as the marker, and the control group underwent conventional arthroscopic popliteal cystectomy. Surgical time of cyst resection, postoperative bruising extent, complication rate, and cyst recurrence rate of the 2 groups were compared.
RESULTS: The MB group had a faster surgical cyst removal time (16.5±1.5 min) than the control group (24.5±1.6 min; P<0.05). The MB group had less postoperative bruising (1 case, 4.5%) than the control group (5 cases, 25%; P<0.05). The surgical results were similar in both groups, with a Lysholm score of 87.23±1.80 in the MB group and 87.23±1.62 (P>0.05) in the control group.
CONCLUSIONS: This study showed that preoperative injection of MB for popliteal cysts before arthroscopic debridement improved cyst localization and ease and accuracy of surgery and reduced operative time, adjacent tissue damage, postoperative complications, and recurrence rate.
Keywords: Arthroscopy, Popliteal Cyst, Methylene Blue, Osteoarthritis, Knee
Introduction
Baker cysts, also known as popliteal cysts, are most commonly found in adults between the ages of 35 and 70 years and are associated with inflammatory joint diseases, such as rheumatoid arthritis and osteoarthritis, or as a result of overuse or injury to the knee joint [1]. They form as a result of the accumulation and extrusion of synovial fluid located between the semimembranosus muscle and the medial head of the gastrocnemius muscle [2].
Severe popliteal cysts are usually treated surgically. The commonly used surgical procedures are open cystectomy and arthroscopic cyst decompression. Open cystectomy is the common treatment for popliteal cysts, but it has some obvious drawbacks. On the one hand, open surgery has a high recurrence rate. On the other hand, it leaves the patient with a huge incision [3]. In recent years, with the rapid development of arthroscopic surgery, the arthroscopic treatment of popliteal cysts has gained wide popularity with its acceptable wound size and almost zero recurrence rate [4]. However, arthroscopic popliteal cysts do not provide a good view for the surgeon. Some little cysts, which are difficult to find precisely, are not guaranteed to be totally eradicated, especially for surgeons without experience. Moving the arthroscope repeatedly to locate popliteal cysts would impair the bordering healthy tissue. To solve this problem, Gu et al used a figure-of-four position and double posteromedial portals to get a better view [5]. However, the identification of arthroscopic popliteal cysts remains challenging during surgery.
Methylene blue (MB) is a fluorescent dye discovered in 1876, which has been commonly used in medical practice [6]. Today, MB is used as a marker or indicator in various surgical techniques [7]. Su et al reported that MB could be used to find and remove tiny metallic foreign bodies embedded in the soft tissues of children [8]. Their results demonstrated that the MB group had much greater success rate, shorter average operation duration, and smaller incision length than the control group. Buyung et al also showed that the surgeon can direct the arthroscopic debridement toward the ganglion stalk with the injection of MB, thus avoiding stripping of unnecessary debridement of uninvolved tissue [9]. These results suggest that MB can be used as an indicator to help the operator quickly localize the lesion during surgery.
Therefore, this retrospective study of 42 patients with popliteal cysts aimed to compare the effects on duration and outcomes of arthroscopic surgical debridement with and without the use of cyst injection with MB.
Material and Methods
RESEARCH DESIGN AND PARTICIPANTS:
Between June 2018 and June 2021, a total of 50 patients requiring arthroscopic popliteal cystectomy for popliteal cysts were enrolled and randomly divided into a trial group and a control group of 25 patients each.
This prospective descriptive study was conducted from June 2018 to June 2021 in the Orthopedic Quadrant of the Tenth People’s Hospital of Tongji University. The hospital ethics committee approved the study. We explained the study methods to all patients or their authorized principals and obtained their written informed consent. Of the original 50 patients, 42 patients were included in the analysis. There was no statistically significant difference in age, sex, and Rauschning and Lindgren classification between the 2 groups (
SURGICAL METHOD:
These patients had arthroscopic surgery in the supine posture under spinal anesthesia with tourniquets. The anterolateral and anteromedial portals were used for routine arthroscopy, intra-articular debridement, such as bone lesion debridement, partial meniscectomy, and synovectomy. The knee was then flexed 90 degrees to establish the posterior medial (PM) portal. A spinal needle was used to locate the entrance of the popliteal cyst, which was often located behind the posterior medial capsular fold of the gastrocnemius muscle (Figure 1A, 1B). After that, the capsule folds were removed with a razor through the PM portal to expose the medial head of the gastrocnemius (Figure 1C) and semembranosus. We then used shaver and basket forceps to totally enlarge the valvular opening and restore 2-way communication.
Afterward, the arthroscope was switched to the PM portal to find the wall of the popliteal cyst along the posterior medial aspect of the medial head of the gastrocnemius muscle (Figure 1D). Then, 2 cm below the initial PM portal, a second PM portal was established (Figure 2) to remove the inner wall of the cyst. Finally, a drainage tube was inserted and pressure bandaged in the popliteal fossa.
The experimental group was operated in almost the same way as the control group. After spinal or general anesthesia, the location of the popliteal cyst was initially determined by combining preoperative imaging and intraoperative physical examination. The cyst cavity was then blindly punctured with a syringe and MB was injected after retraction of a slightly yellow clarified fluid (Figure 3). The same arthroscopic debridement as in the control group was performed. After exposing the medial head of the gastrocnemius muscle, the blue cyst stained by MB could be clearly seen (Figure 4), and the same treatment as in the control group was performed.
POSTOPERATIVE REHABILITATION AND FOLLOW-UP:
Ice packs were applied on the first postoperative day, and routine anti-inflammatory, pain-relieving, and edema elimination treatments were given for 2 to 3 days. The popliteal fossa needed to be bandaged with pressure for 2 weeks to prevent the formation of hematomas and new masses in this area. The patient could walk and perform activities, such as quadriceps muscle training and knee flexion, after surgery. Partial weight-bearing, such as wearing a brace, was allowed for 6 weeks after surgery. Removal of the brace and full weight-bearing activities were allowed 6 weeks after surgery. Quadriceps isometric exercises and knee flexion were continued for about 3 months after surgery. Patients were followed up with MRI 6 months after surgery to check whether the popliteal cyst disappeared, decreased in size, or recurred (Figure 5).
EVALUATION PARAMETERS:
All patients were followed up, and the presence of vascular nerve injury and recurrence cases were recorded; the visual analogue scale (VAS) pain scores and Lysholm scores of patients before and 12 months after surgery were recorded to assess the clinical efficacy of surgical treatment.
STATISTICAL METHODS:
Statistical analysis was performed using SPSS version 18.0. The data were presented as mean±standard deviation. Comparisons were done by one-way ANOVA, with least significant difference post hoc tests or chi-square tests with chi-square partitioning.
Results
GENERAL PATIENT INFORMATION:
The control group included 7 men and 13 women, aged 65±9.79 years, and duration of disease was 28±11.31 months. The MB group included 8 men and 14 women, age 64.73±7.75 years, and disease duration 22±5.61 months. All patients in the 2 groups underwent preoperative MRI of the knee joint and lateral radiographs of the knee joint to assess the relationship between the cyst and the surrounding tissues and the presence of other lesions in the joint. The follow-up period was 6 months, and during the follow-up period, 42 patients were followed up (a total of 8 patients were lost to follow-up).
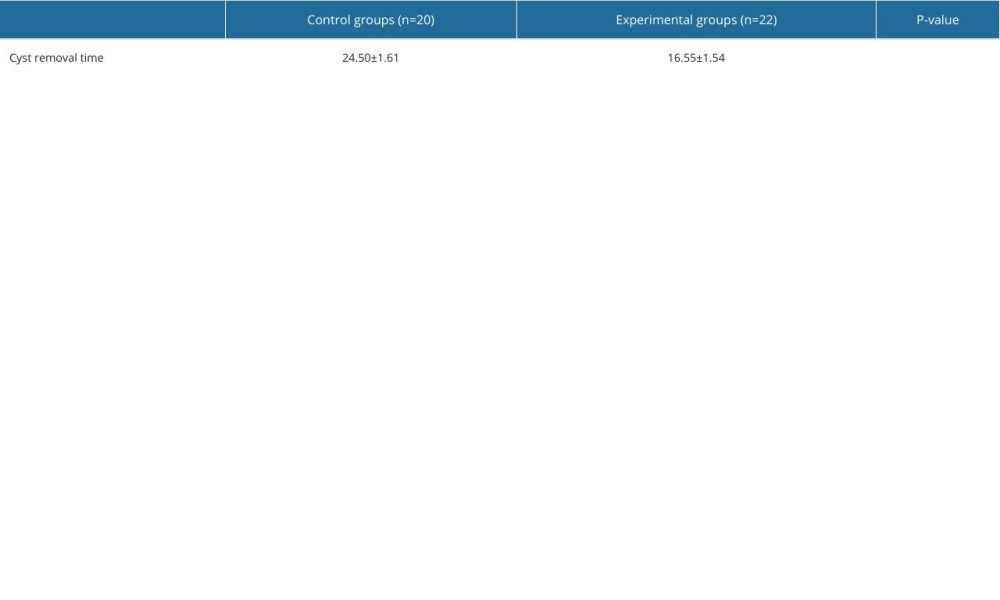
SURGERY TIME OF CYST RESECTION:
After arthroscopic treatment of knee osteoarthritis, a re-timing of the time used for cyst removal was performed. Table 1 shows the comparison of cyst clearance time in the control and experimental groups. In the control group, the surgical time was longer because the operator performed the cyst removal arthroscopically based on his own experience, and his judgment of the extent of the cyst may have been incorrect. The mean operative time in the control group was 24.50±1.61 min. In the MB group, after marking with MB, the operator could see the cyst more clearly, and a significantly shorter operation time was achieved. In the MB group, the average operative time was 16.55±1.54 min. Compared with that of the control group, the surgery time was significantly shorter in the MB group (P<0.01; Table 1).
POST-OPERATIVE BRUISING:
In the control group, the operator may have misjudged the extent of the cyst and probably damaged the surrounding small veins during resection, and there were 5 patients with a bruising area greater than 1 cm2, including 1 patient with a postoperative bruising area greater than 5 cm2. In the control group, the incidence of postoperative bruising was 25%. In the MB group, the extent of the cyst had been marked by MB, and there was less possibility of damaging the surrounding tissues; therefore, there was 1 postoperative bruising area greater than 1 cm2, and no large bruising occurred. In the MB group, the incidence of postoperative bruising was 4.5%.
INCIDENCE OF COMPLICATIONS:
In both groups, there was no vascular or nerve damage, and the patients had normal foot artery pulsation, and normal lower limb function, and no postoperative numbness.
RECURRENCE RATE OF CYSTS:
In the control group, the popliteal cysts may not be completely removed, due to the operator’s poor identification of the cysts under arthroscopy, especially the smaller ones. In the control group, there was 1 case of cyst recurrence seen on a knee MRI 6 months after surgery. The recurrence rate in the control group was 5%. In the MB group, the extent of the cyst was stained with MB and was more easily excised by cutting the base, and there was no recurrence in the MB group (
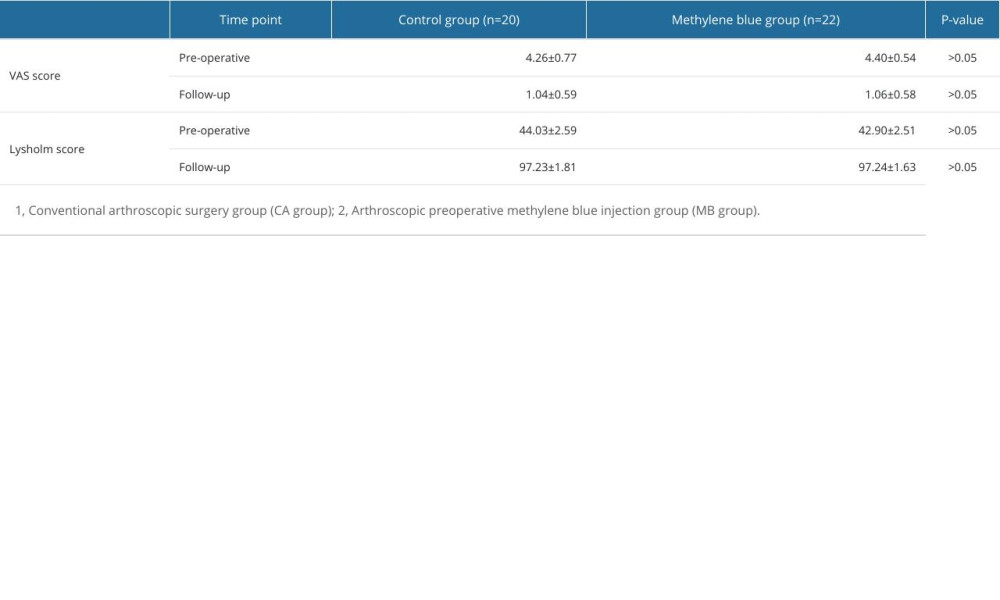
POSTOPERATIVE VAS PAIN AND LYSHOLM SCORES AT 6 MONTHS:
Table 2 shows the follow-up results and comparison between the 2 groups of patients. The VAS scores and Lysholm scores in both groups were significantly lower than before surgery (P<0.01). However, there were no statistically significant differences between the 2 groups in VAS and Lysholm scores (P>0.05)
Discussion
Arthroscopic popliteal cyst excision is a minimally invasive, low-complication, and feasible procedure. Injection of MB into the popliteal cyst makes it easier for the surgeon to differentiate. During the procedure, the surgeon can greatly improve speed and accuracy. However, there were no significant differences in postoperative bruising, complications, recurrence rates, or VAS and Lysholm scores at 6 months after surgery.
A horizontal fissure-like structure exists between the medial head of the gastrocnemius and the bursa of the semimembranosus and the joint cavity. The structure is not obvious in early childhood but becomes longer with age. Marti-Bonmati et al studied the incidence of popliteal cysts by MRI. They found 145 popliteal cysts in 382 knees (38%), and there was a significant association between knee effusion and popliteal cysts (
Depending on the conditions related to the patient’s knee and popliteal cysts, the doctor will establish different treatments. For some patients with mild clinical symptoms, untreated or simple supportive therapy can relieve the associated symptoms and shrink, or even regress, the cyst. For patients with significant pain and restricted joint mobility, ultrasound-guided aspiration of joint fluid and injection of glucocorticoids into the joint cavity and cysts has minimal risk but can easily lead to cyst recurrence [13]. Alternatively, cyst puncture and intracapsular injection of the sclerosing agent are also effective treatment options [14]. For patients for whom non-surgical therapy has been unsuccessful for 6 months, open surgery or arthroscopic surgery is a choice [15]. Traditional open surgery creates a large field of vision that could properly locate and remove the cyst’s body; however, the damage to healthy tissue is huge, often resulting in a protracted postoperative recovery period for patients and a high recurrence rate [16].
Arthroscopic treatment is effective in treating popliteal cysts and significantly reduces tissue damage. According to one study, arthroscopy can be an effective treatment for popliteal cysts. At a mean follow-up time of 24 months, the VAS pain score decreased from 8.8 (±3.5) before surgery to 3.1 (±1.4) after surgery, and the Lysholm Knee Function Score improved from 43.6 (±5.3) to 87.5 (±3.7) [4]. This is consistent with the results we have gathered. However, the operator’s vision was severely limited [17]. Anatomically, between the semitendinosus and medial head of the gastrocnemius muscle are various nerves and blood vessels. To cut the cyst more accurately, without damaging the surrounding blood vessels and nerves, the surgeon has to rotate their device frequently to better position the popliteal cyst, which inevitably injures the surrounding healthy tissue. Therefore, the importance of precise arthroscopic differentiation of the cyst is key to the entire procedure, and its importance cannot be overemphasized.
MB has been widely used as a dye to assist in the localization of lesions during surgery [8,9,18]. MB, for example, has been used as a marker for localizing lesions in the treatment of patients undergoing precise hepatic resections [19], the thoracoscopic pulmonary nodule procedure [20], microscopic apical surgery [21], detection of mucosal perforations during laparoscopic surgery [22], finding and removing microscopic metallic foreign bodies in the soft tissue of children [8], and complete removal of the carpal ganglion capsule in children [9]. MB can quickly mark the margins of the cyst, eliminating the need for the surgeon to laboriously find it. With the help of MB, the surgical procedure is simplified and the operation time is significantly shortened, therefore reducing the harm to healthy tissues caused by surgery. Similarly, cysts can also be more easily identified by arthroscopy when stained with MB. According to our results, arthroscopy was also easier for identifying and removing cysts after staining with MB, with a removal time of 24.50 (±1.61) min in the control group and 16.55 (±1.54) min in the MB group (
MB is a low-cost, non-toxic chemical with few adverse effects. MB has a long history of use and safety, which has led to widespread interest. In addition, it is required in very small amounts and causes no harm to either the patient or the surgeon. We did not find any postoperative diseases related to MB in our 42 patients during the follow-up. Thus, our findings suggest that the use of MB to label popliteal cysts is a straightforward strategy to reduce surgical injury while achieving promising results.
The limitations of this study are the small number of cases and the short follow-up period. The next study needs a large-sample prospective study and long-term follow-up. MB is also not indicated for patients who are allergic.
Conclusions
The use of MB as a marker to remove popliteal cysts has several advantages. Localization is accurate, and intraoperative damage to surrounding healthy tissue is reduced. Shortened operative time helps minimize the risk of damage to surrounding tissues. This approach has clear benefits for clearing popliteal cysts.
Figures
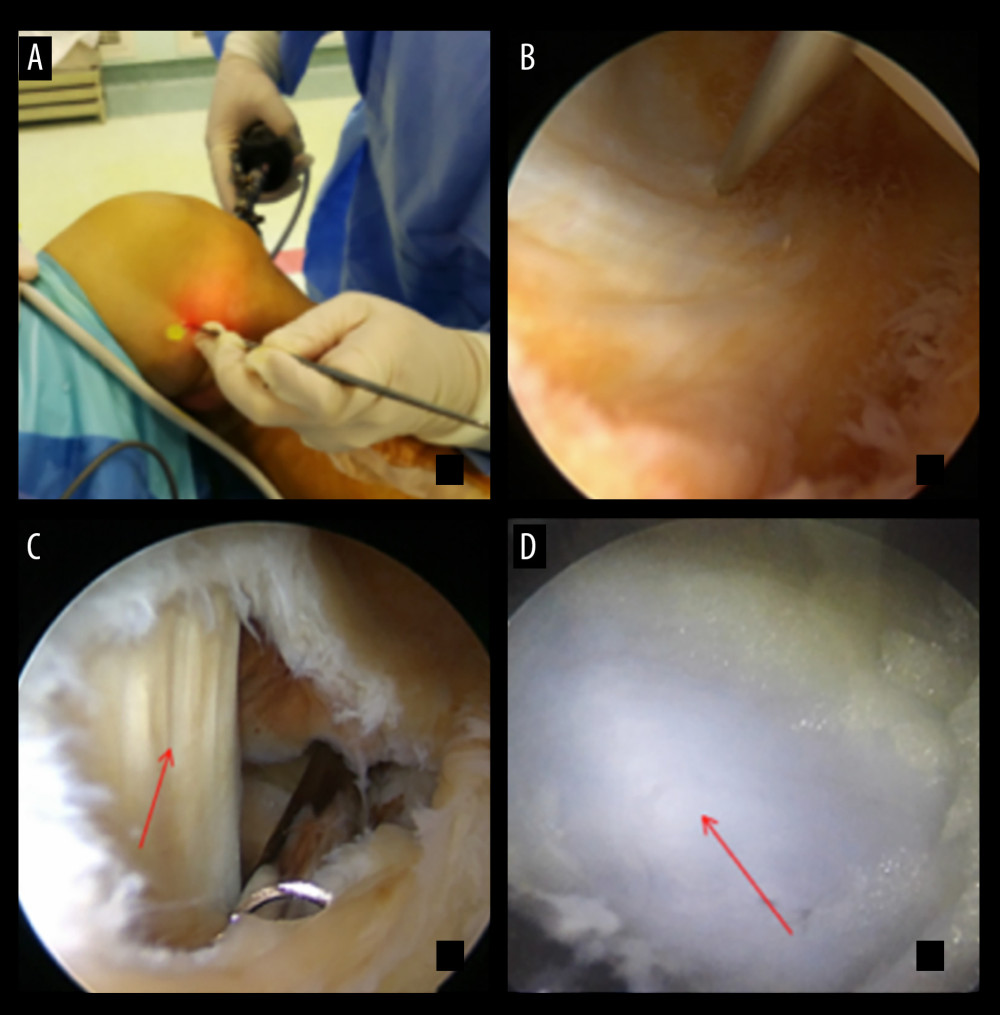 Figure 1. Surgical procedure. (A, B) The posterior medial approach is established under the knee quadratus. (C) The medial head of the gastrocnemius muscle (arrow) and semembranosus is exposed after excision of the capsular crease. (D) The popliteal cyst (arrow) can be exposed posteriorly medial to the medial head of the gastrocnemius muscle, which is very faint and difficult to see without methylene blue staining.
Figure 1. Surgical procedure. (A, B) The posterior medial approach is established under the knee quadratus. (C) The medial head of the gastrocnemius muscle (arrow) and semembranosus is exposed after excision of the capsular crease. (D) The popliteal cyst (arrow) can be exposed posteriorly medial to the medial head of the gastrocnemius muscle, which is very faint and difficult to see without methylene blue staining.  Figure 2. Arthroscopic resection of popliteal cyst with high posterior medial approach and low posterior medial approach.
Figure 2. Arthroscopic resection of popliteal cyst with high posterior medial approach and low posterior medial approach. 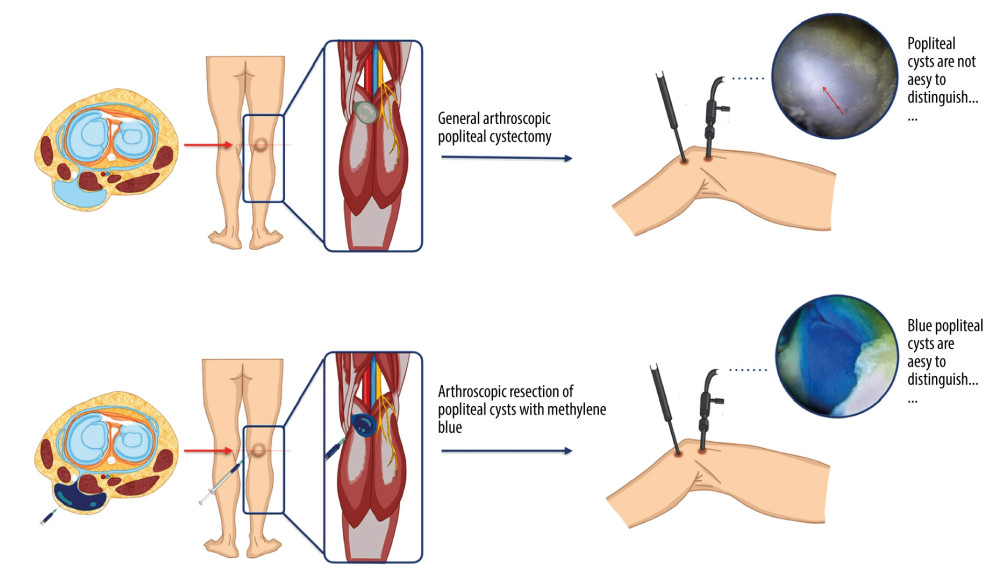 Figure 3. Schematic illustration of methylene blue staining.
Figure 3. Schematic illustration of methylene blue staining. 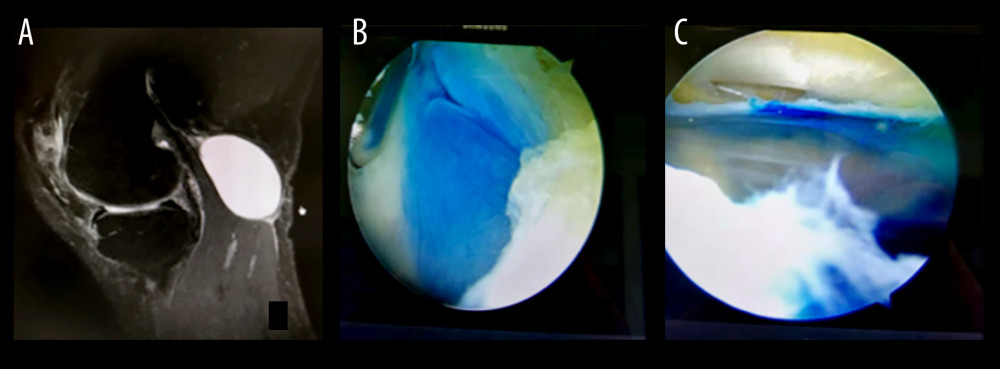 Figure 4. Arthroscopic visualization of popliteal cysts after methylene blue staining. (A) MRI shows a popliteal cyst located posteriorly within the medial head of the gastrocnemius muscle. (B) Methylene blue staining after drainage of the cystic fluid shows the extent of the cyst wall, which can be clearly identified, thus enabling complete excision of the cyst wall to reduce the recurrence rate of the cyst. (C) Performance after excision of the medial wall of the popliteal cyst.
Figure 4. Arthroscopic visualization of popliteal cysts after methylene blue staining. (A) MRI shows a popliteal cyst located posteriorly within the medial head of the gastrocnemius muscle. (B) Methylene blue staining after drainage of the cystic fluid shows the extent of the cyst wall, which can be clearly identified, thus enabling complete excision of the cyst wall to reduce the recurrence rate of the cyst. (C) Performance after excision of the medial wall of the popliteal cyst. 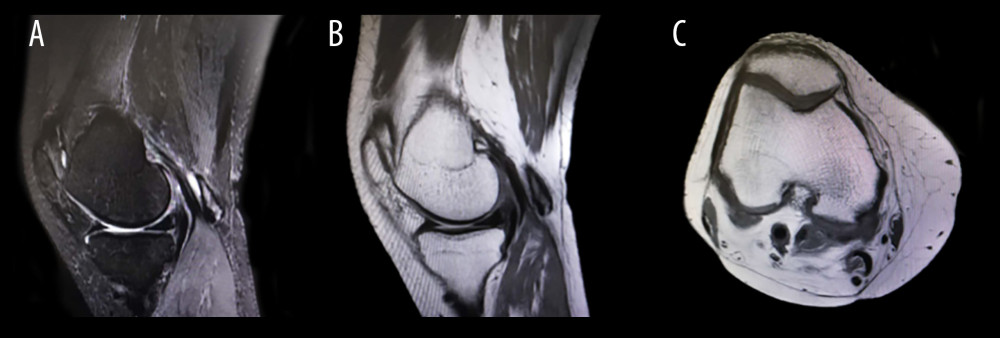 Figure 5. Patient (same patient as in Figure 4) 6 months postoperative review MRI. (A) Sagittal T2-weighted image moderate signal shows that the original popliteal cyst has disappeared. (B) Sagittal T1-weighted image low signal with void at the original popliteal cyst. (C) Coronal T1-weighted image shows the disappearance of the popliteal cyst.
Figure 5. Patient (same patient as in Figure 4) 6 months postoperative review MRI. (A) Sagittal T2-weighted image moderate signal shows that the original popliteal cyst has disappeared. (B) Sagittal T1-weighted image low signal with void at the original popliteal cyst. (C) Coronal T1-weighted image shows the disappearance of the popliteal cyst. 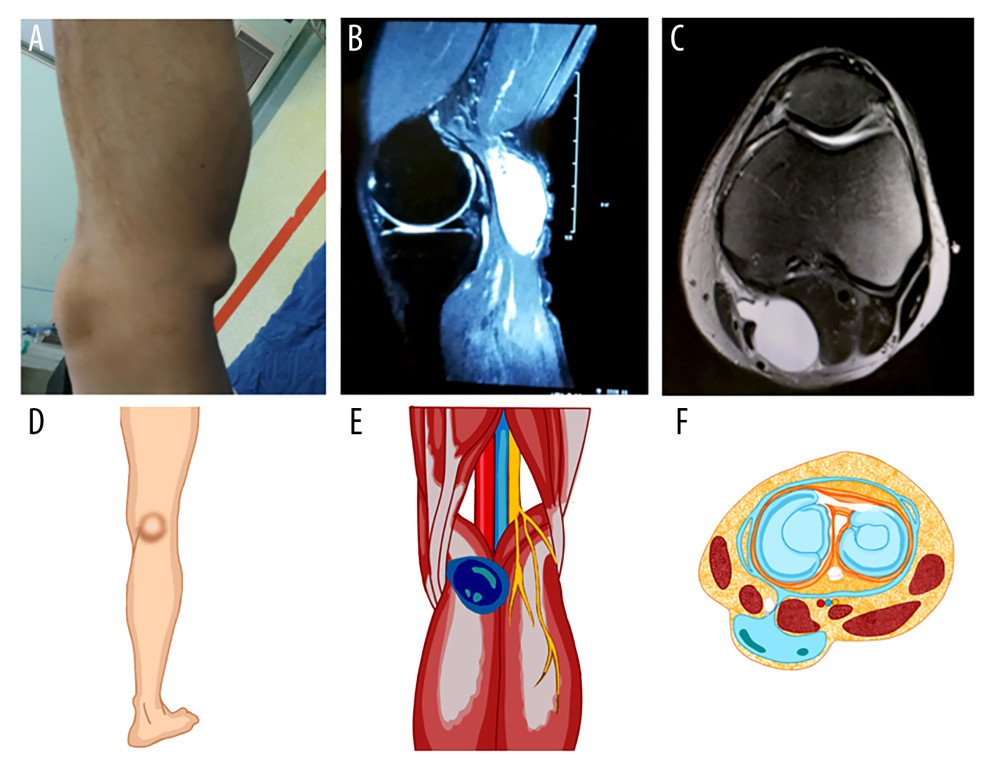 Figure 6. Popliteal cyst: (A) A significant cyst is seen in the posterior popliteal fossa. (B) MRI T2-weighted image shows a homogeneous high signal mass in the posterior part of the popliteal fossa. (C) Horizontal MRI shows that the popliteal cyst is located between the medial head of the gastrocnemius muscle and the semimembranosus muscle. (D–F) Schematic diagram of location of popliteal cysts, anatomical structures and horizontal planes.
Figure 6. Popliteal cyst: (A) A significant cyst is seen in the posterior popliteal fossa. (B) MRI T2-weighted image shows a homogeneous high signal mass in the posterior part of the popliteal fossa. (C) Horizontal MRI shows that the popliteal cyst is located between the medial head of the gastrocnemius muscle and the semimembranosus muscle. (D–F) Schematic diagram of location of popliteal cysts, anatomical structures and horizontal planes. References
1. Abate M, Di Carlo L, Di Iorio A, Salini V, Baker’s cyst with knee osteoarthritis: Clinical and therapeutic implications: Med Princ Pract, 2021; 30(6); 585-91
2. Herman AM, Marzo JM, Popliteal cysts: A current review: Orthopedics, 2014; 37(8); e678-84
3. Yang B, Wang F, Lou Y, A comparison of clinical efficacy between different surgical approaches for popliteal cyst: J Orthop Surg Res, 2017; 12(1); 158
4. Jiang J, Ni L, Arthroscopic internal drainage and cystectomy of popliteal cyst in knee osteoarthritis: J Orthop Surg Res, 2017; 12(1); 182
5. Gu H, Bi Q, Chen J, Arthroscopic treatment of popliteal cyst using a figure-of-four position and double posteromedial portals: Int Orthop, 2019; 43(6); 1503-8
6. Cwalinski T, Polom W, Marano L, Methylene blue-current knowledge, fluorescent properties, and its future use: J Clin Med, 2020; 9(11); 3538
7. Nedu ME, Tertis M, Cristea C, Georgescu AV, Methylene blue and proflavine as intraarterial marker for functional perforazome-comparative study: J Pers Med, 2021; 11(2); 147
8. Su Y, Nan G, Using methylene blue as a marker to find and remove tiny metallic foreign bodies embedded in the soft tissues of children: A randomised controlled trial: Int J Surg, 2016; 29; 43-48
9. Lee BJ, Sawyer GA, Dasilva MF, Methylene blue-enhanced arthroscopic resection of dorsal wrist ganglions: Tech Hand Up Extrem Surg, 2011; 15(4); 243-46
10. Martí-Bonmatí L, Mollá E, Dosdá R, MR imaging of Baker cysts – prevalence and relation to internal derangements of the knee: Magma, 2000; 10(3); 205-10
11. Sanchez JE, Conkling N, Labropoulos N, Compression syndromes of the popliteal neurovascular bundle due to Baker cyst: J Vasc Surg, 2011; 54(6); 1821-29
12. Fritschy D, Fasel J, Imbert JC, The popliteal cyst: Knee Surg Sports Traumatol Arthrosc, 2006; 14(7); 623-28
13. Van Nest DS, Tjoumakaris FP, Smith BJ, Popliteal cysts: A systematic review of nonoperative and operative treatment: JBJS Rev, 2020; 8(3); e0139
14. Cakmakci E, Celebi I, Ozal ST, Can ultrasonography-guided aspiration and steroid injection treat reflux venous blood flow around symptomatic Baker’s cysts? Our short-term experience: Radiol Med, 2017; 122(9); 690-95
15. Zhou XN, Li B, Wang JS, Bai LH, Surgical treatment of popliteal cyst: A systematic review and meta-analysis: J Orthop Surg Res, 2016; 11; 22
16. You C, Cheng Z, Xia Y, Comparison of arthroscopic internal drainage and open excision for the treatment of popliteal cysts: BMC Musculoskelet Disord, 2022; 23(1); 732
17. Brazier BG, Sudekum SA, DeVito PM, Dodds JA, Arthroscopic treatment of popliteal cysts: Arthrosc Tech, 2018; 7(11); e1109-e14
18. Graves RM, Sands KC, Making a cost-effective contrast bone cement with or without antibiotics, using aqueous methylene blue for easy cement removal in revision and primary total joint arthroplasty: Orthopedics, 2007; 30(10); 825-27
19. Diana M, Usmaan H, Legnèr A, Novel laparoscopic narrow band imaging for real-time detection of bile leak during hepatectomy: Proof of the concept in a porcine model: Surg Endosc, 2016; 30(7); 3128-32
20. Lin CY, Chang CC, Huang LT, Computed tomography-guided methylene blue localization: Single vs. multiple lung nodules: Front Med (Lausanne), 2021; 8; 661956
21. Qian WH, Hong J, Xu PCAnalysis of the possible causes of endodontic treatment failure by inspection during apical microsurgery treatment: Shanghai Kou Qiang Yi Xue, 2015; 24(2); 206-9 [in Chinese]
22. Vegunta RK, Rawlings AL, Jeziorczak PM, Methylene blue: A simple marker for intraoperative detection of gastroduodenal perforations during laparoscopic pyloromyotomy: Surg Innov, 2010; 17(1); 11-13
Figures
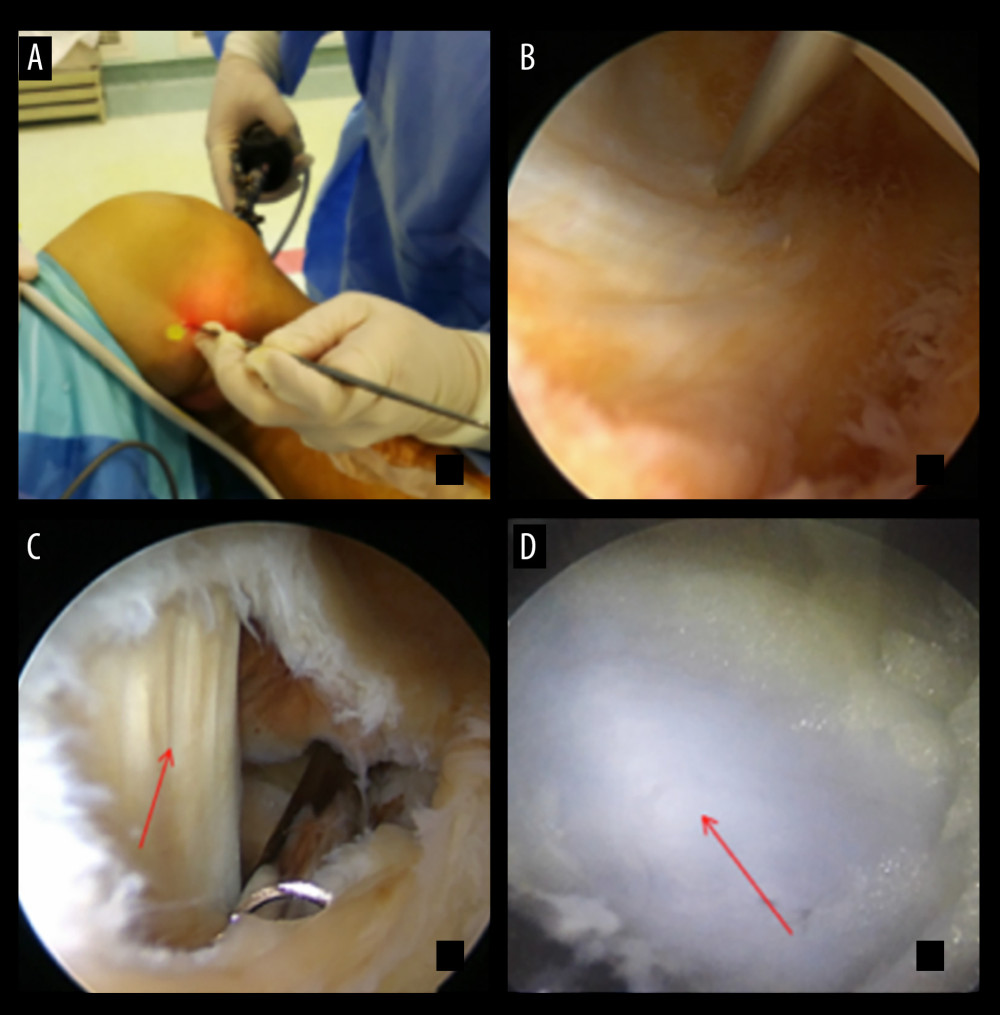 Figure 1. Surgical procedure. (A, B) The posterior medial approach is established under the knee quadratus. (C) The medial head of the gastrocnemius muscle (arrow) and semembranosus is exposed after excision of the capsular crease. (D) The popliteal cyst (arrow) can be exposed posteriorly medial to the medial head of the gastrocnemius muscle, which is very faint and difficult to see without methylene blue staining.
Figure 1. Surgical procedure. (A, B) The posterior medial approach is established under the knee quadratus. (C) The medial head of the gastrocnemius muscle (arrow) and semembranosus is exposed after excision of the capsular crease. (D) The popliteal cyst (arrow) can be exposed posteriorly medial to the medial head of the gastrocnemius muscle, which is very faint and difficult to see without methylene blue staining. Figure 2. Arthroscopic resection of popliteal cyst with high posterior medial approach and low posterior medial approach.
Figure 2. Arthroscopic resection of popliteal cyst with high posterior medial approach and low posterior medial approach.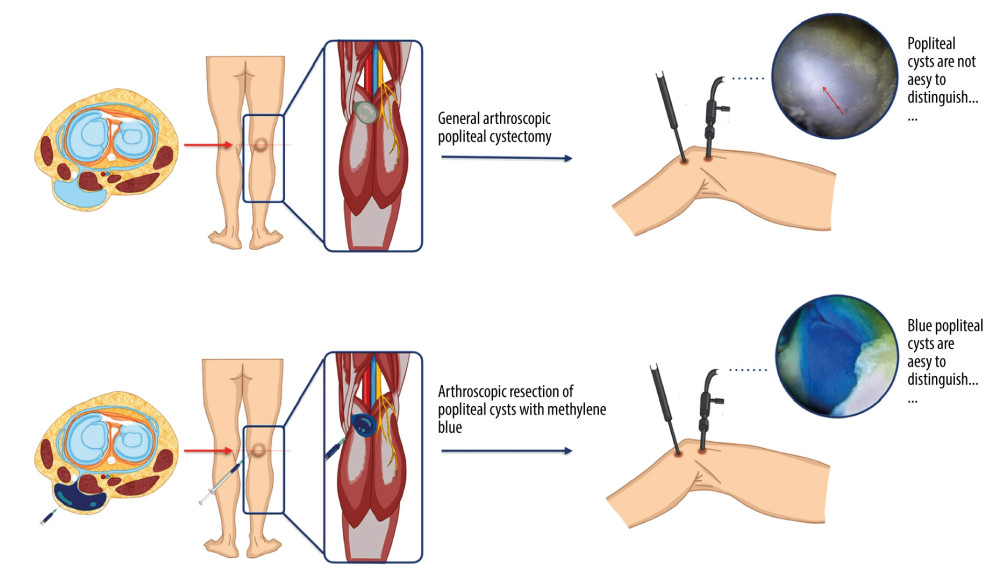 Figure 3. Schematic illustration of methylene blue staining.
Figure 3. Schematic illustration of methylene blue staining.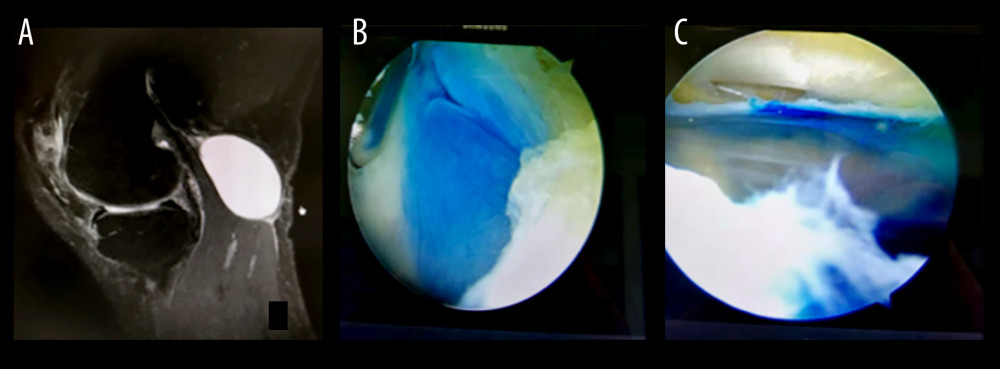 Figure 4. Arthroscopic visualization of popliteal cysts after methylene blue staining. (A) MRI shows a popliteal cyst located posteriorly within the medial head of the gastrocnemius muscle. (B) Methylene blue staining after drainage of the cystic fluid shows the extent of the cyst wall, which can be clearly identified, thus enabling complete excision of the cyst wall to reduce the recurrence rate of the cyst. (C) Performance after excision of the medial wall of the popliteal cyst.
Figure 4. Arthroscopic visualization of popliteal cysts after methylene blue staining. (A) MRI shows a popliteal cyst located posteriorly within the medial head of the gastrocnemius muscle. (B) Methylene blue staining after drainage of the cystic fluid shows the extent of the cyst wall, which can be clearly identified, thus enabling complete excision of the cyst wall to reduce the recurrence rate of the cyst. (C) Performance after excision of the medial wall of the popliteal cyst.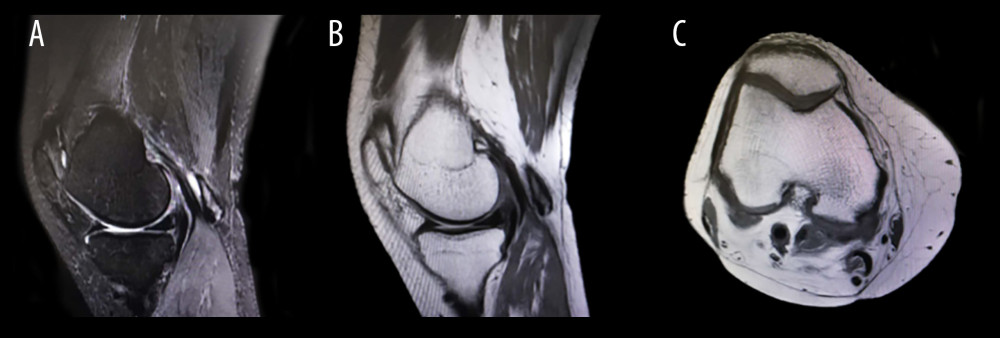 Figure 5. Patient (same patient as in Figure 4) 6 months postoperative review MRI. (A) Sagittal T2-weighted image moderate signal shows that the original popliteal cyst has disappeared. (B) Sagittal T1-weighted image low signal with void at the original popliteal cyst. (C) Coronal T1-weighted image shows the disappearance of the popliteal cyst.
Figure 5. Patient (same patient as in Figure 4) 6 months postoperative review MRI. (A) Sagittal T2-weighted image moderate signal shows that the original popliteal cyst has disappeared. (B) Sagittal T1-weighted image low signal with void at the original popliteal cyst. (C) Coronal T1-weighted image shows the disappearance of the popliteal cyst.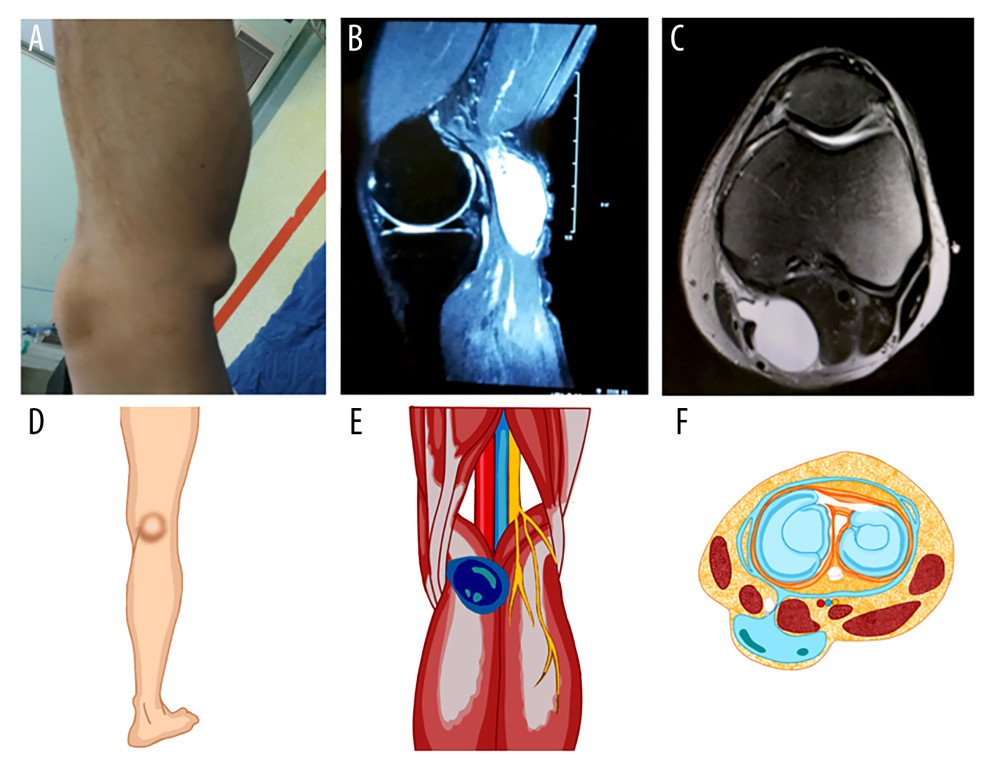 Figure 6. Popliteal cyst: (A) A significant cyst is seen in the posterior popliteal fossa. (B) MRI T2-weighted image shows a homogeneous high signal mass in the posterior part of the popliteal fossa. (C) Horizontal MRI shows that the popliteal cyst is located between the medial head of the gastrocnemius muscle and the semimembranosus muscle. (D–F) Schematic diagram of location of popliteal cysts, anatomical structures and horizontal planes.
Figure 6. Popliteal cyst: (A) A significant cyst is seen in the posterior popliteal fossa. (B) MRI T2-weighted image shows a homogeneous high signal mass in the posterior part of the popliteal fossa. (C) Horizontal MRI shows that the popliteal cyst is located between the medial head of the gastrocnemius muscle and the semimembranosus muscle. (D–F) Schematic diagram of location of popliteal cysts, anatomical structures and horizontal planes. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952