18 April 2024: Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser Lithotripsy
Xiaoling Chen1ABCDEF, Libin He1ABCD, Xiao Yu1ABCD, Yuqing Bo1ADEF, Lei Yu1ACD, Qiumei Chen1CDEF, Zhuoer Zhao1AG*DOI: 10.12659/MSM.942836
Med Sci Monit 2024; 30:e942836
Abstract
BACKGROUND: Patients with urolithiasis often undergo transurethral ureteroscopic holmium laser lithotripsy, a procedure that can be affected by perioperative thermal management. This study examines the impact of compound thermal insulation management on patient recovery and comfort during transurethral ureteroscopic holmium laser lithotripsy.
MATERIAL AND METHODS: In this study, 551 patients who underwent transurethral ureteroscopic holmium laser lithotripsy from April 2019 to December 2022 were randomly assigned to either an observation group (n=276) or control group (n=275). Both groups received routine surgical care, with the observation group additionally receiving compound thermal insulation management. We recorded and compared perioperative body temperature changes, anesthetic resuscitation indicators (bispectral index recovery time, extubation time, fully awake time, Postanesthesia Care Unit retention time), comfort level (General Comfort Questionnaire), and quality of life (Nottingham Health Profile). We also compared the incidence of complications.
RESULTS: There was no significant difference in body temperature between groups at the start surgery. However, the observation group showed significantly higher temperatures during and at the end of surgery. Anesthetic resuscitation indicators were significantly better in the observation group. Both groups showed improved comfort and quality of life after surgery, with more significant improvements in the observation group. The observation group also had a lower incidence of complications, such as hypothermia and rigor.
CONCLUSIONS: Compound thermal insulation management during transurethral ureteroscopic holmium laser lithotripsy improved perioperative temperature maintenance, accelerated postoperative recovery, reduced complication rates, and enhanced patient comfort and quality of life.
Keywords: Clinical Nursing Research, Hypothermia, Lithotripsy
Introduction
Urolithiasis is a common surgical disease, and lithiasis is most likely to occur in the human urinary system [1]. The incidence of lithiasis is increasing annually, and the development of lithiasis has markedly reduced patients’ quality of life. Surgery is the first choice for clearing lithiasis [2]. Traditional surgery is more harmful to patients and can cause complications, and has been gradually replaced by minimally invasive surgery [3]. Holmium laser lithotripsy, currently the main therapy for urolithiasis, causes less trauma to patients after surgery and has a high success rate, allowing it to be widely applied in multiple hospitals [4]. Nevertheless, because large areas of exposed skin are needed during surgery and anesthesia and perfusion need to be performed at low temperatures, hypothermia and complications can occur, which seriously affect patients’ postoperative recovery [5].
When the body temperature is lower than 35°C, the body’s oxygen consumption decreases, which easily causes dysfunction of the body and reduced blood flow in the skin, weakens immune function, reduces patient resistance, reduces platelet count, reduces the activity of blood clotting substances, activates the fibrinolysis system, and causes prolonged bleeding [6]. Simultaneously, blood flow is slow, blood viscosity increases, metabolism is reduced, and the excretion of anesthetic drugs in the body is prolonged under a low-temperature state, which leads to a delay in patient recovery time after surgery [7], affecting patient prognosis and recovery [8].
In conventional surgical nursing, patients are often maintained at room temperature by wrapping the patient’s exposed skin with a surgical towel, adjusting the indoor temperature, and performing other external adjustment methods [9]. Although this method can exert a certain effect, the internal temperature drop caused by the use of massive amounts of low-temperature liquids, such as flushing fluid and infusion fluid, during surgery cannot be avoided; this approach cannot reduce the occurrence of hypothermic events or other hypothermic complications during surgery, affecting patients’ quality of life and prognosis [10]. Thus, appropriate insulation measures should be taken during surgery [11]. Thermal insulation is effective for preventing inadvertent perioperative hypothermia from both internal and external perspectives [10]. To maintain the patient’s external temperature, several strategies are employed: pre-adjusting the operating room temperature, using thermal insulation blankets, and wrapping exposed skin areas with surgical towels [10]. Internally, the temperature of fluids administered to the patient is carefully regulated to ensure warmth, contributing to the stability of the patient’s core temperature during surgery [12,13].
In this study, we evaluated the effects of compound thermal insulation management intervention on patients receiving transurethral ureteroscopic holmium laser lithotripsy by assessing perioperative body temperature dynamics, anesthesia recovery, perioperative comfort, quality of life, and incidence of perioperative complications.
Material and Methods
PARTICIPANT SELECTION AND GROUPING:
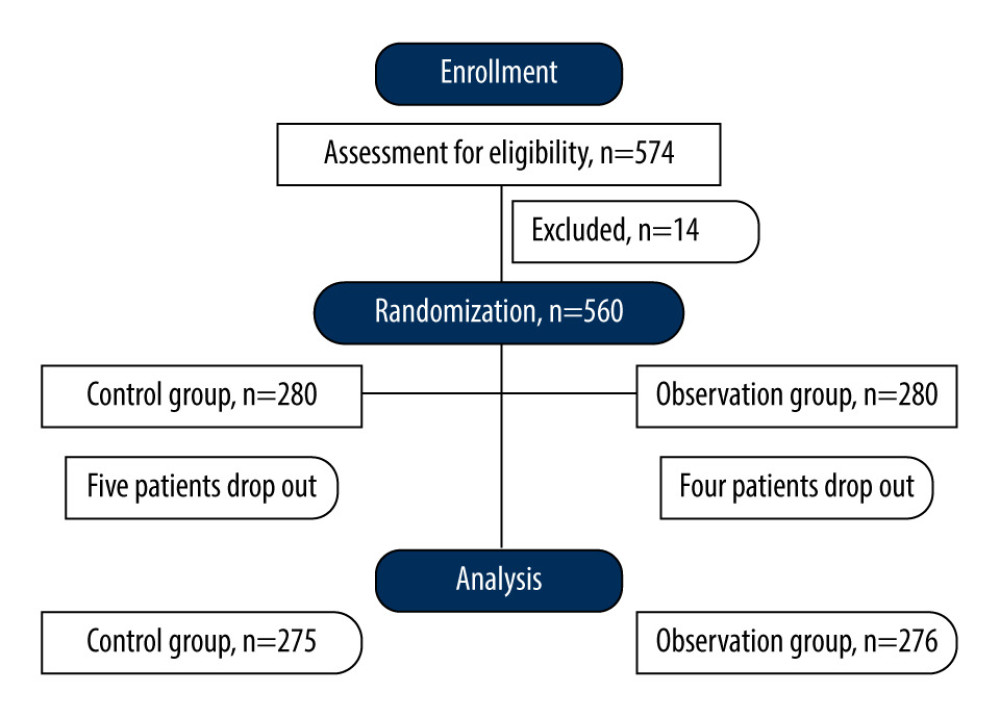
A total of 560 patients with urolithiasis who underwent transurethral ureteroscopic holmium laser lithotripsy at our hospital from April 2019 to December 2022 were included in our research. The sample size was determined using the G.power tool. The patients were randomly divided into an observation group (n=280) and control group (n=280) using a random number table. Patients who had urolithiasis, were aged 18 to 75 years, were independently conscious, and provided consent for the study were included. Patients with an operation time >90 min, acute infection, solitary kidney, coexisting ureteric disease (tumor or stricture), pregnancy, cardiovascular or pulmonary comorbidities, serious mental diseases, or malignancies were excluded. Patients who dropped out of the study were also excluded.
CLINICAL PROCEDURES AND NURSING INTERVENTIONS:
The patients in both groups received routine surgical nursing, such as disinfection of instruments, inspection and verification of needed drugs, wrapping of the patient’s exposed skin, except for the operation site, with a surgical towel, and monitoring of the patient’s heart rate and blood pressure. The observation group received additional compound insulation. Before surgery, the temperature was adjusted to 22°C to 24°C, and the perfusate, flushing fluid, and other liquids needed for the surgery were heated and kept in the incubator to maintain the temperature at 37°C. The patients were kept warm before reaching the operating room. The operating bed was covered with a thermal insulation blanket. During surgery, patient temperature was monitored regularly. The patients were warmed in a timely manner, and the temperature was reported to the doctor if it was declining. During the surgery, the skin from the operation area was uncovered to reduce exposure; the blood, flushing fluids and other stains on the patients’ skin were removed in a timely manner; and the volatilization and heat absorption of the fluids were reduced. A wet-heat exchanger was used to ensure that the temperature of the inhaled gas was consistent during intubation. After surgery, the temperature control system of the Postanesthesia Care Unit (PACU) was adjusted to the appropriate temperature in advance. A thermal insulation blanket was used to maintain the temperature when patients were discharged from the operating room until they were sent to the PACU. The operation time was monitored and noted.
OUTCOME MEASURES AND EVALUATION CRITERIA:
This study rigorously evaluated a range of outcomes to comprehensively understand the effects of transurethral ureteroscopic holmium laser lithotripsy on patients with urolithiasis. Our evaluation criteria were designed to capture clinical and patient-reported outcomes, ensuring a holistic assessment of the procedure’s efficacy and impact on patient well-being. The parameters of perioperative temperature changes and anesthetic resuscitation indices were measured and analyzed. The body temperature changes in both groups at each time point (when entering the operating room, at anesthesia induction, beginning of operation, 60 min during operation, and end of operation) during the perioperative period were recorded and compared. The anesthetic resuscitation indices (bispectral index [BIS] recovery time, extubation time, fully awake time, and PACU retention time) during the perioperative period were compared between the 2 groups.
PATIENT COMFORT AND QUALITY OF LIFE:
The comfort levels of both groups before and 3 days after surgery were compared with the General Comfort Questionnaire (GCQ) [14]. Comfort was scored on 4 aspects, namely physiology, psychology, society, and environment, for a total possible score of 100 points. Higher scores suggested better comfort levels. The quality of life in both groups was compared with the Nottingham Health Profile (NHP) [15]. NHP scores reflect quality of life by evaluating physical function, sleep, pain, and other issues from the perspective of patients. Lower scores suggest better quality of life.
PERIOPERATIVE COMPLICATIONS:
We also tracked and compared the occurrence of specific complications during the perioperative period in both groups. This included conditions such as hypothermia, dysphoria, and rigor.
STATISTICAL ANALYSIS:
SPSS 20.0 software was used for the data analysis. Measurement data are expressed as χ̄±s, and an independent
Results
DEMOGRAPHIC AND BASELINE CHARACTERISTICS:
Analysis of the demographic data revealed no significant discrepancies between the 2 study cohorts. The 2 groups were comparable in terms of sex distribution and mean age; the control group included 195 men and 80 women (mean age: 47.49±13.75 years), and the observation group included 204 men and 72 women (mean age: 47.51±13.80 years) (Table 1). Four patients in the observation group dropped out, and 5 patients in the control group dropped out (Figure 1); consequently, 276 patients in the observation group and 275 patients in the control group were included. The average operation time in the control group was 64.56±15.34 min, whereas that in the observation group was 68.56±13.34 min. In the observation group, there were 84 patients had left-sided urolithiasis, 92 right-sided, and 100 bilateral, and a stone diameter of 1.84±0.35 cm. In the control group, there were 90 patients with left-sided urolithiasis, 91 right-sided, and 94 bilateral, and a stone diameter of 1.78±0.41 cm (Table 1). The general data of the 2 groups were comparable (P>0.05).
PERIOPERATIVE BODY TEMPERATURE DYNAMICS:
Initial assessments of body temperature upon entering the operating room and at the time of anesthesia induction revealed no significant differences between the 2 groups, with mean temperatures essentially equivalent. However, as the surgical procedure progressed, the observation group displayed a notable increase in mean body temperature, particularly at the beginning of the operation (36.90±0.20°C vs 36.70±0.30°C), 60 min into the operation (36.80±0.30°C vs 35.90±0.20°C), and at the operation’s conclusion (36.80±0.20°C vs 35.70±0.30°C), compared with those of the control group. These elevations were statistically significant (all P<0.001), suggesting effective thermoregulation strategies or interventions within the observation group (Table 2).
ANESTHESIA RECOVERY INDICATORS:
Postoperative recovery metrics indicated a more expedited recovery process for the observation group across all measured indicators. Specifically, the observation group experienced shorter mean BIS recovery times (15.34±1.67 min vs 16.51±2.24 min), earlier extubation (24.37±6.21 min vs 29.55±7.24 min), faster return to full consciousness (43.57±10.24 min vs 51.68±13.47 min), and reduced PACU retention times (52.34±11.82 min vs 62.83±13.49 min) than did the control group (all P<0.001). These findings suggest enhanced recovery efficiencies or possible anesthetic management benefits in the observation group (Table 3).
PERIOPERATIVE COMFORT AND QUALITY OF LIFE ASSESSMENTS:
Evaluations of patient comfort and quality of life, as gauged through GCQ and NHP scores, revealed interesting dynamics. Both groups demonstrated an increase in mean GCQ scores postoperatively, with the observation group showing a more substantial increase (79.43±5.19 vs 75.74±5.28). Conversely, the mean NHP score decreased in both groups, indicating a perceived improvement in health status, with a more pronounced reduction observed in the observation group (46.75±5.74 vs 50.43±5.86) (all P<0.001). These trends can reflect the positive impact of the procedural or pain management protocols used in the observation group (Table 4).
INCIDENCE OF PERIOPERATIVE COMPLICATIONS:
The observation group exhibited a significantly lower incidence of common perioperative complications. Notably, compared with those in the control group, the rates of hypothermia (5.43% vs 18.18%), rigor (3.99% vs 8.36%), and overall complications (9.06% vs 27.27%) were substantially lower. These reductions in complication rates (all P<0.001, except for rigor P=0.033) underscore the potential efficacy of the preventative measures or interventions adopted in the observation group during the perioperative period (Table 5).
Discussion
This study contributes to the growing body of research on thermal management during surgical procedures, particularly in the context of transurethral ureteroscopic holmium laser lithotripsy [16–18]. Our study revealed that the observation group, which received the compound thermal insulation management, demonstrated significant improvements in maintaining body temperature during surgery. This was evident from the marked increase in body temperature at various stages of the operation, compared with that of the control group. Furthermore, recovery times, including BIS recovery time, extubation time, fully awake time, and PACU retention time, were significantly reduced in the observation group. These results corroborate with previous findings suggesting that maintaining normothermia can prevent complications such as thrombocytopenia, prolonged bleeding, and delayed metabolism of anesthetic drugs, thereby enhancing postoperative recovery [7,19].
In addition to physiological benefits, our study also demonstrated improvements in patient comfort and quality of life. The observation group showed a higher GCQ score and lower NHP score after surgery, indicating enhanced comfort and quality of life. These findings are consistent with the notion that an appropriate intraoperative temperature can minimize stress responses and improve overall surgical outcomes [20,21].
Comparatively, traditional methods of maintaining normothermia, such as the use of surgical towels and adjusting room temperature, have been found to be less effective, particularly in surgeries involving large amounts of low-temperature liquids [9,10]. Our study adds to this body of knowledge by demonstrating the superiority of a compound thermal insulation approach, which addresses internal and external temperature regulation.
This study, while comprehensive in its approach, has certain limitations that should be acknowledged. First, the generalizability of the findings may be limited due to the specific patient population from a single institution, raising questions about the applicability of these findings to broader demographic groups. Additionally, as a single-center study, the results could reflect the unique practices and patient characteristics of the particular hospital, which might not be representative of other settings. Another notable limitation is the duration of follow-up; a longer observation period could reveal more about the long-term effects and sustainability of the thermal insulation management technique. There is also a possibility that unmeasured confounding factors were not accounted for in the study, which could have influenced the outcomes. These limitations highlight areas for further research and suggest caution when extrapolating the study’s findings to different contexts or populations.
Conclusions
This study demonstrated that compound thermal insulation management effectively maintains perioperative temperature, accelerates anesthetic resuscitation, and enhances postoperative recovery in patients receiving transurethral ureteroscopic holmium laser lithotripsy. By reducing the incidence of complications associated with hypothermia, this method significantly improves patient comfort and quality of life. Given its cost-effectiveness and potential to positively influence patient outcomes, compound thermal insulation management is highly recommended for operating room nursing staff practices. This approach could have a transformative impact on clinical protocols, elevating the standard of patient care in surgical settings.
Tables
Table 1. General data in the 2 groups.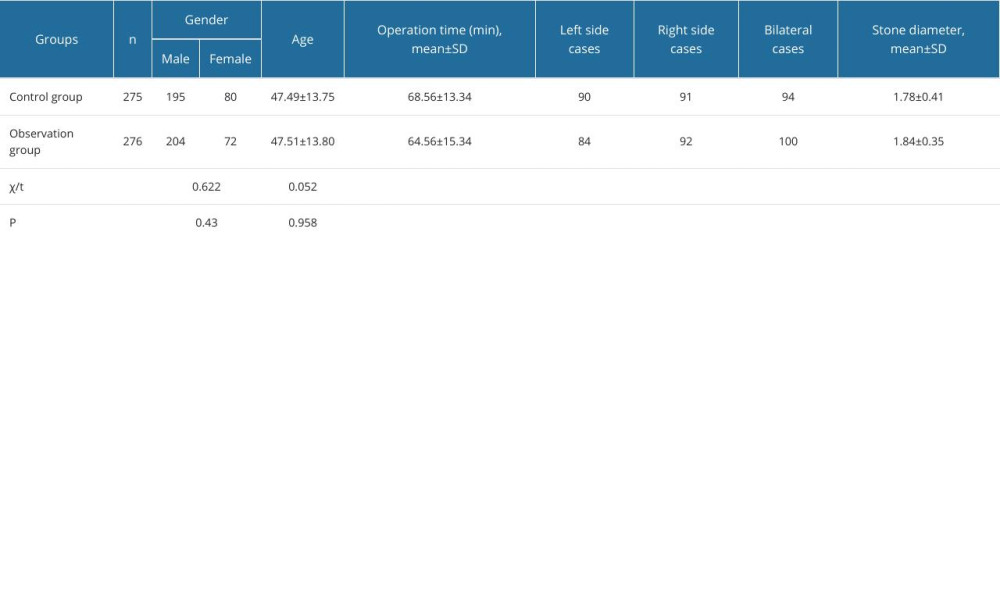 Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).
Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).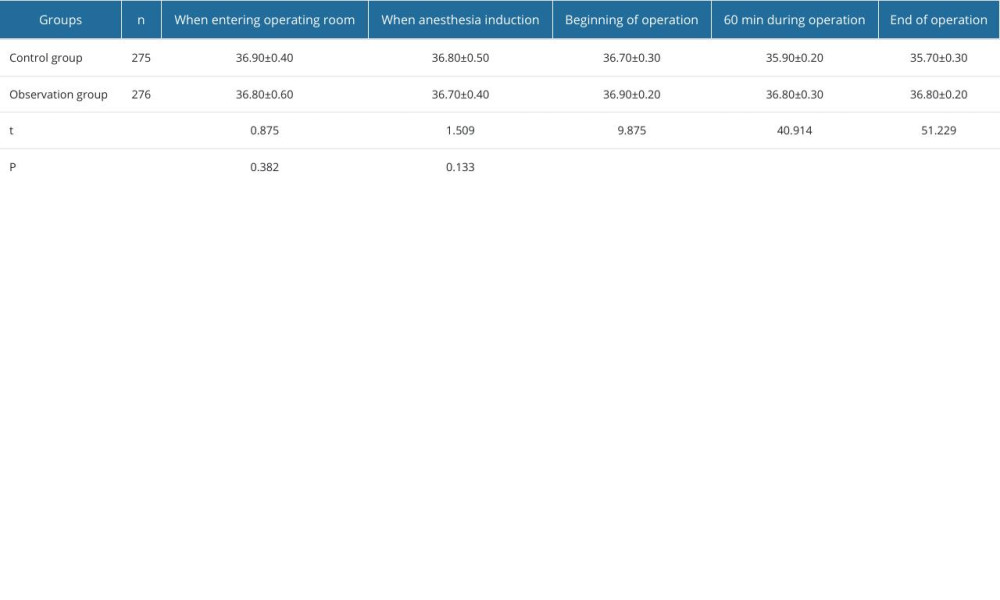 Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).
Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).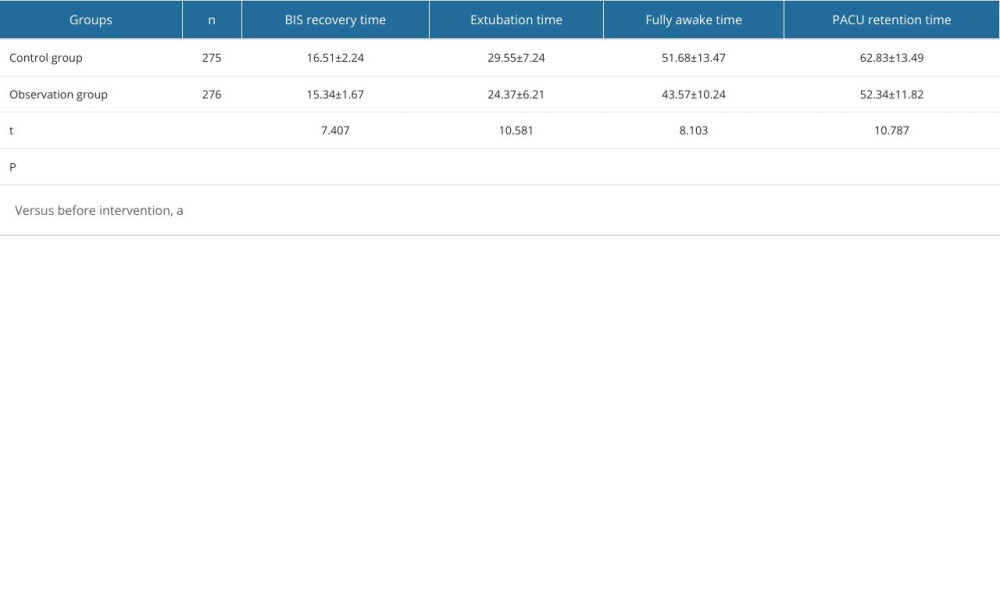 Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).
Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).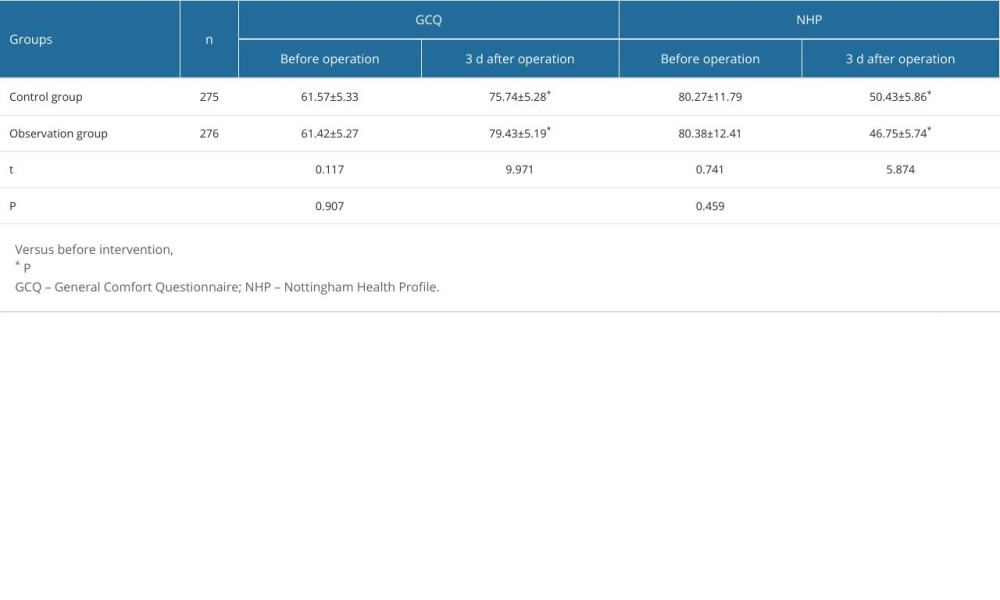 Table 5. Complications in the 2 groups [n (%)].
Table 5. Complications in the 2 groups [n (%)].![Complications in the 2 groups [n (%)].](https://jours.isi-science.com/imageXml.php?i=t5-medscimonit-30-e942836.jpg&idArt=942836&w=1000)
References
1. Chimenz R, Cannavo L, Viola V, Pediatric urolithiasis: J Biol Regul Homeost Agents, 2019; 33(5 Suppl 1); 39-44
2. Cassini MF, Cologna AJ, Andrade MF, Lithiasis in 1,313 kidney transplants: Incidence, diagnosis, and management: Transplant Proc, 2012; 44(8); 2373-75
3. Galli P, Ceva A, Foletti JM, Salivary gland lithiasis recurrence after minimally-invasive surgery: Incidence, risk factors and prevention: Laryngoscope, 2021; 131(4); 794-99
4. Liang H, Liang L, Yu Y, Thermal effect of holmium laser during ureteroscopic lithotripsy: BMC Urol, 2020; 20(1); 69
5. Ye WX, Ren LG, Chen L, Inverted Y ureteral duplication with an ectopic ureter and multiple urinary calculi: A case report: World J Clin Cases, 2022; 10(4); 1326-32
6. Coiffard B, Diallo AB, Mezouar S, A tangled threesome: Circadian rhythm, body temperature variations, and the immune system: Biology (Basel), 2021; 10(1); 65
7. Ruetzler K, Kurz A, Consequences of perioperative hypothermia: Handb Clin Neurol, 2018; 157; 687-97
8. Shao L, Pang N, Yan P, Control of body temperature and immune function in patients undergoing open surgery for gastric cancer: Bosn J Basic Med Sci, 2018; 18(3); 289-96
9. Nieh HC, Su SF, Meta-analysis: Effectiveness of forced-air warming for prevention of perioperative hypothermia in surgical patients: J Adv Nurs, 2016; 72(10); 2294-314
10. Alderson P, Campbell G, Smith AF, Thermal insulation for preventing inadvertent perioperative hypothermia: Cochrane Database Syst Rev, 2014(6); CD009908
11. Hegarty J, Walsh E, Burton A, Nurses’ knowledge of inadvertent hypothermia: AORN J, 2009; 89(4); 701-4
12. Bolt LB, Stannard D, Thermal insulation for preventing inadvertent perioperative hypothermia: J Perianesth Nurs, 2015; 30(5); 427-29
13. Chen S, Qian W, Feng J, Thermal insulation during recovery from anesthesia: A systematic review and meta-analysis: Ann Palliat Med, 2021; 10(11); 11394-402
14. Gois JA, Freitas KS, Kolcaba K, Mussi FC, Cross-cultural adaptation of the General Comfort Questionnaire to Brazilian patients with myocardial infarction: Rev Bras Enferm, 2018; 71(6); 2998-3005
15. Chmaj-Wierzchowska K, Rzymski P, Wojciechowska M, Health-related quality of life (Nottingham Health Profile) in patients with endometriomas: Correlation with clinical variables and self-reported limitations: Arch Med Sci, 2020; 16(3); 584-91
16. Urits I, Jones MR, Orhurhu V, A comprehensive update of current anesthesia perspectives on therapeutic hypothermia: Adv Ther, 2019; 36(9); 2223-32
17. Insler SR, Sessler DI, Perioperative thermoregulation and temperature monitoring: Anesthesiol Clin, 2006; 24(4); 823-37
18. Hildebrand F, Giannoudis PV, van Griensven M, Pathophysiologic changes and effects of hypothermia on outcome in elective surgery and trauma patients: Am J Surg, 2004; 187(3); 363-71
19. Zhang J, Deng L, Wang X, Effect of forced-air warming blanket on perioperative hypothermia in elderly patients undergoing laparoscopic radical resection of colorectal cancer: Ther Hypothermia Temp Manag, 2022; 12(2); 68-73
20. Bach V, Libert JP, Hyperthermia and heat stress as risk factors for sudden infant death syndrome: A narrative review: Front Pediatr, 2022; 10; 816136
21. Sessler DI, Perioperative thermoregulation and heat balance: Lancet, 2016; 387(10038); 2655-64
Tables
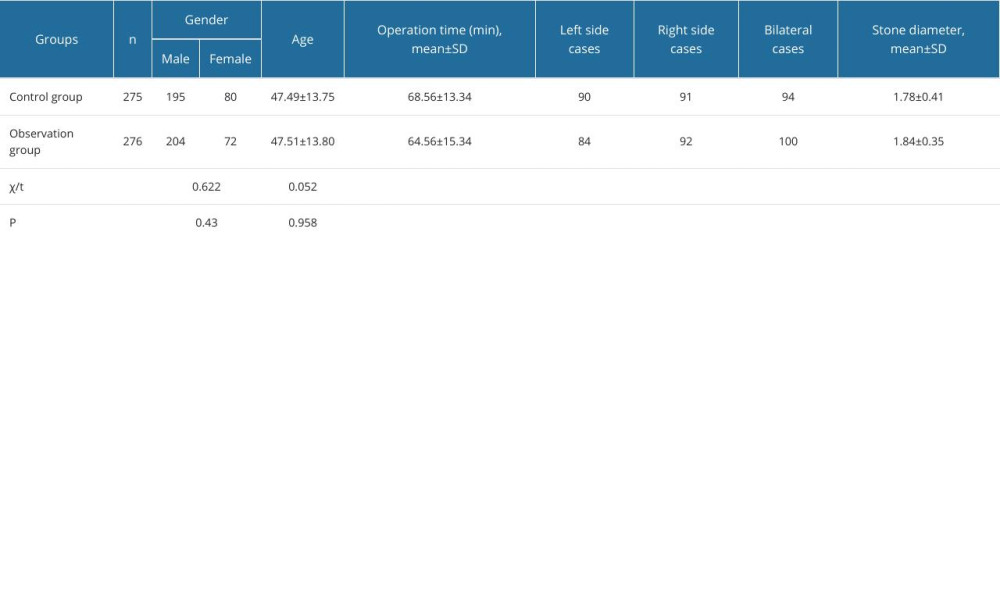 Table 1. General data in the 2 groups.
Table 1. General data in the 2 groups.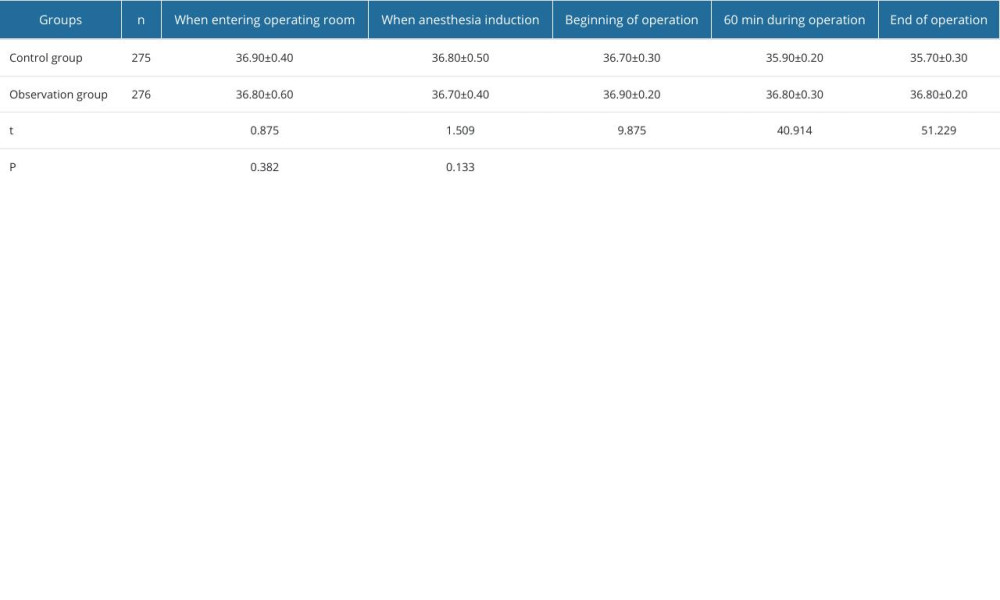 Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).
Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).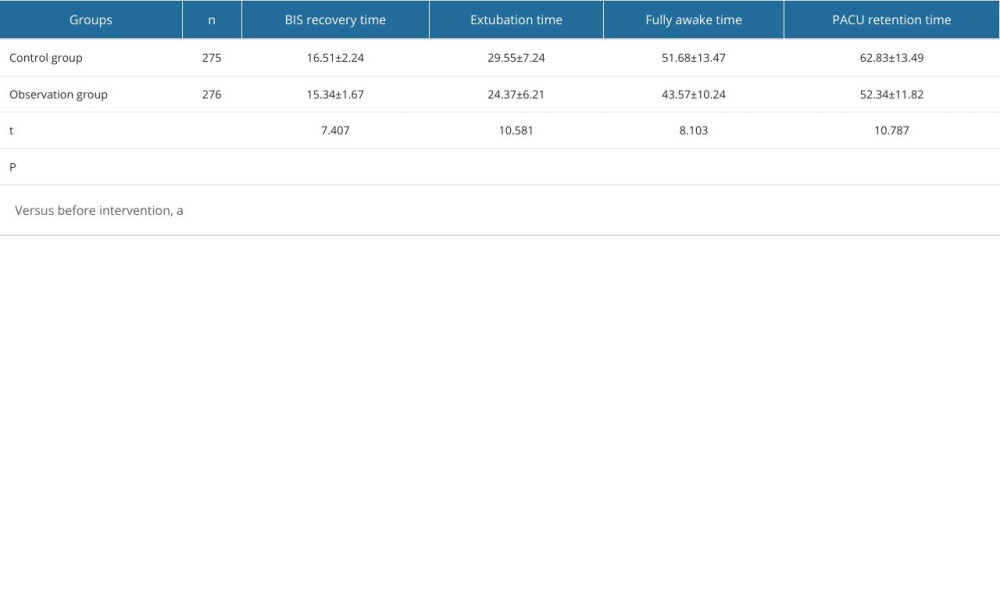 Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).
Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).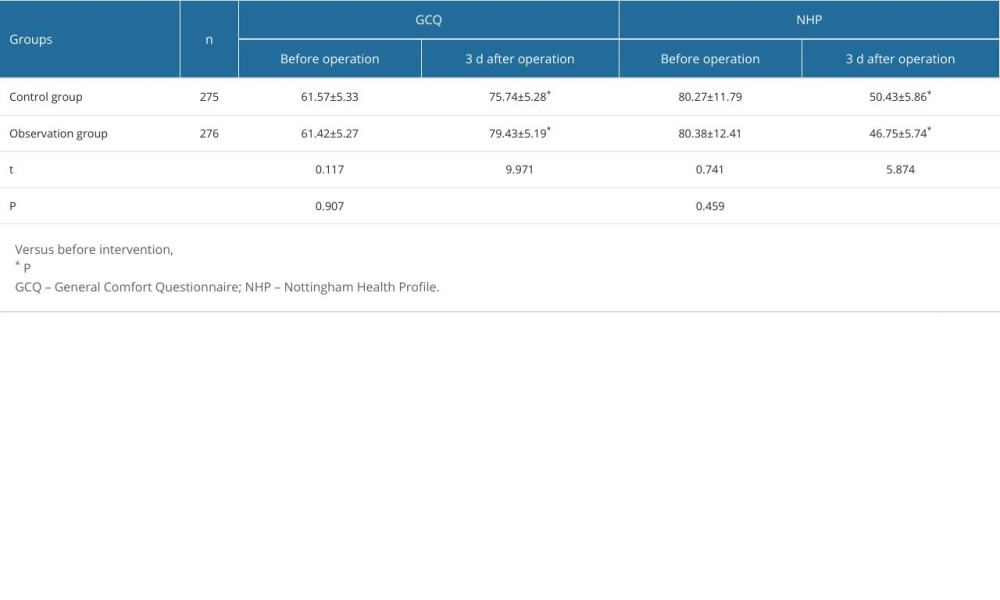 Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).
Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).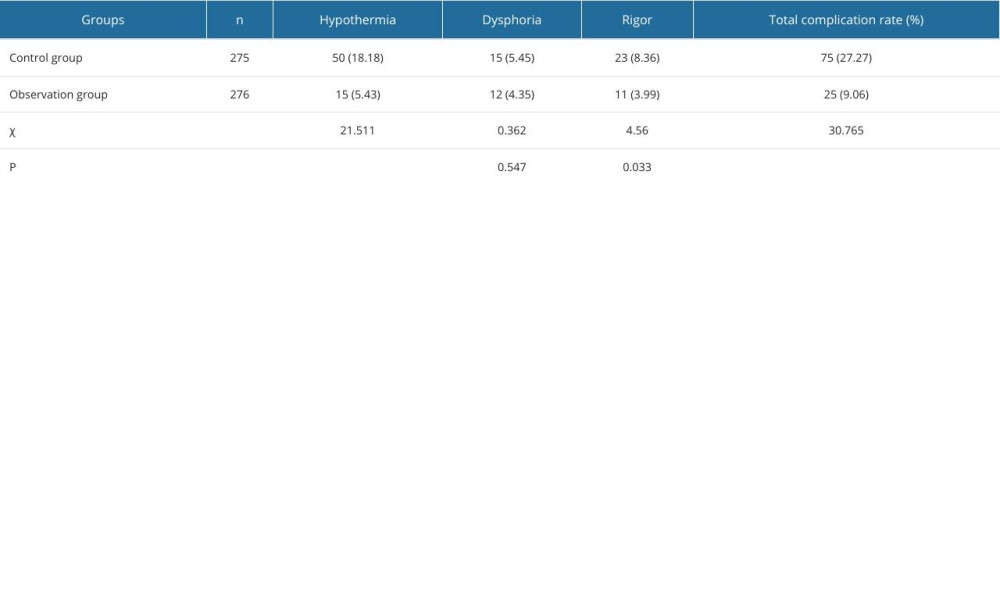 Table 5. Complications in the 2 groups [n (%)].
Table 5. Complications in the 2 groups [n (%)].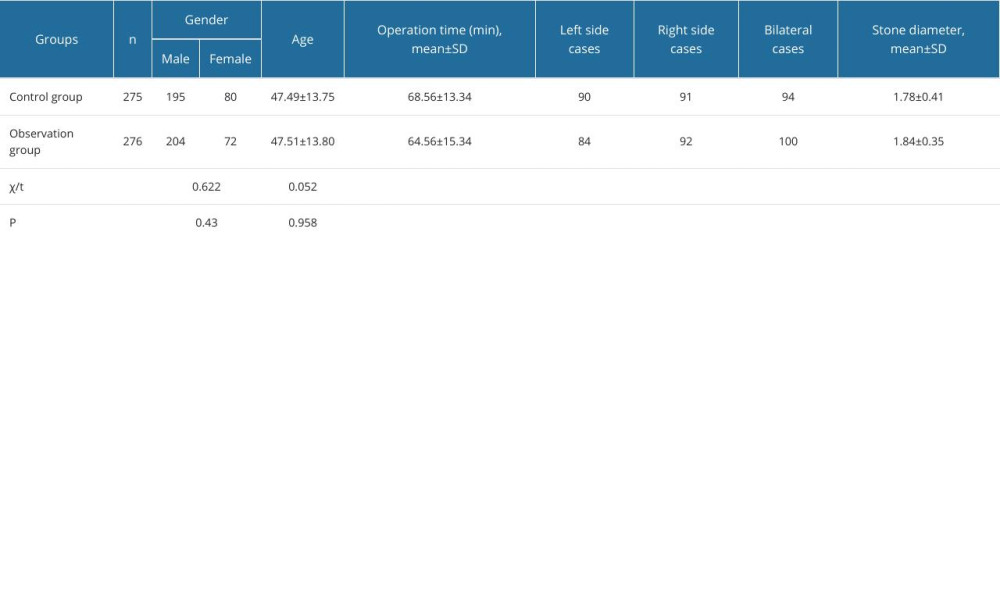 Table 1. General data in the 2 groups.
Table 1. General data in the 2 groups.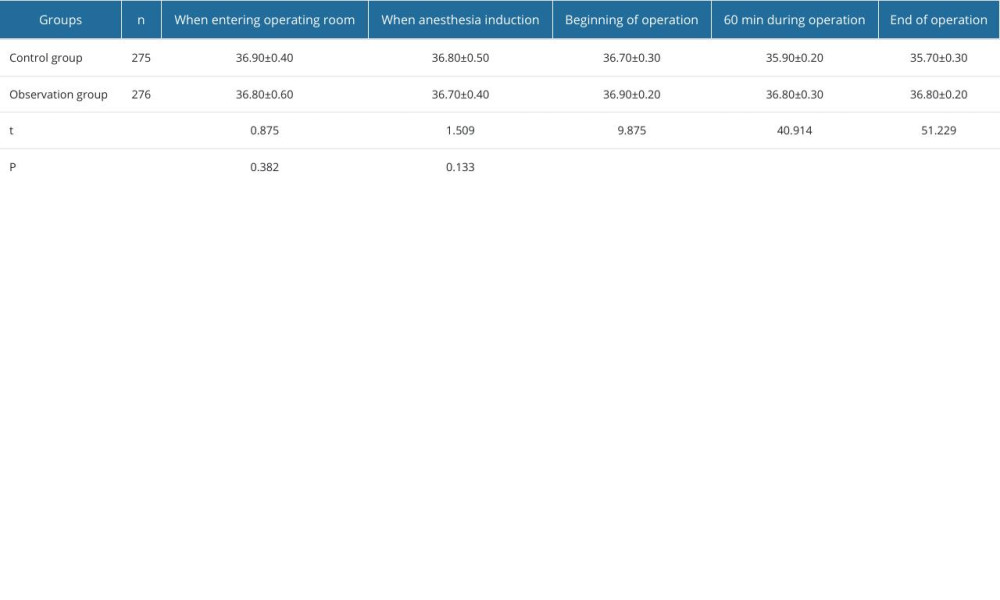 Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).
Table 2. Body temperature at different time points in the 2 groups (χ̄±s, °C).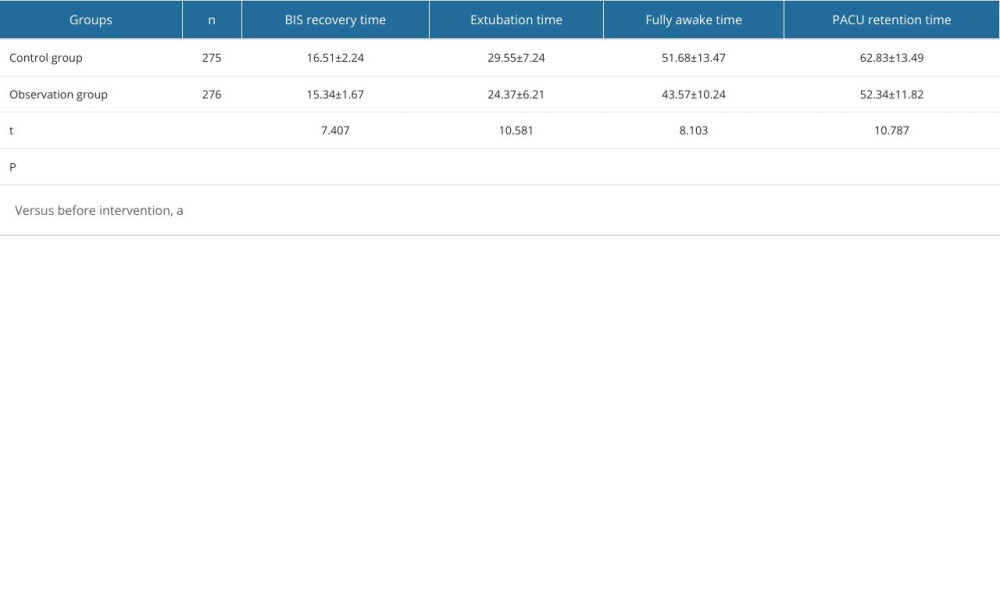 Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).
Table 3. Anesthesia resuscitation indicators in the 2 groups (χ̄±s, min).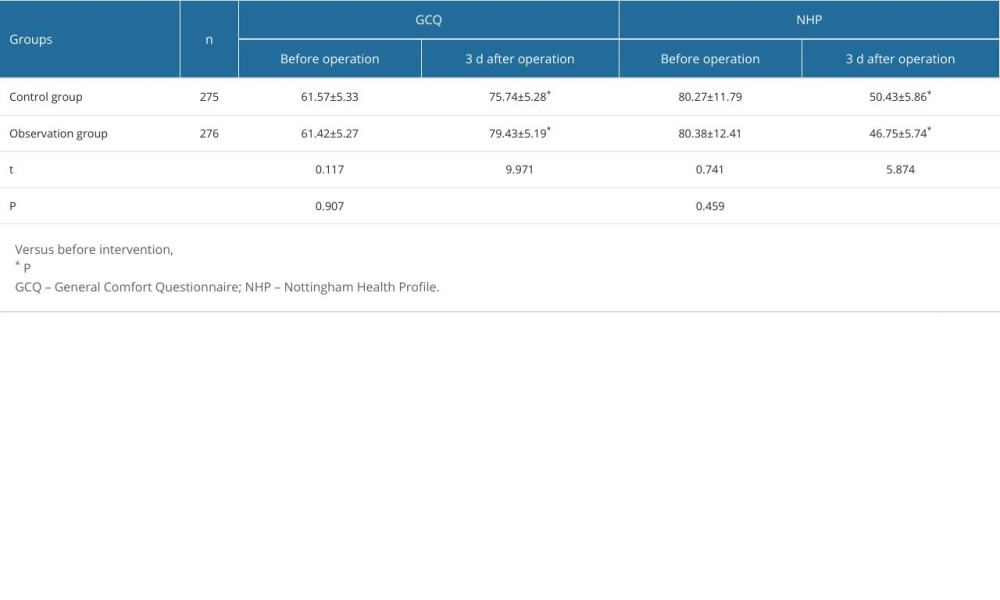 Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).
Table 4. General Comfort Questionnaire and Nottingham Health Profile scores in the 2 groups (χ̄±s, point).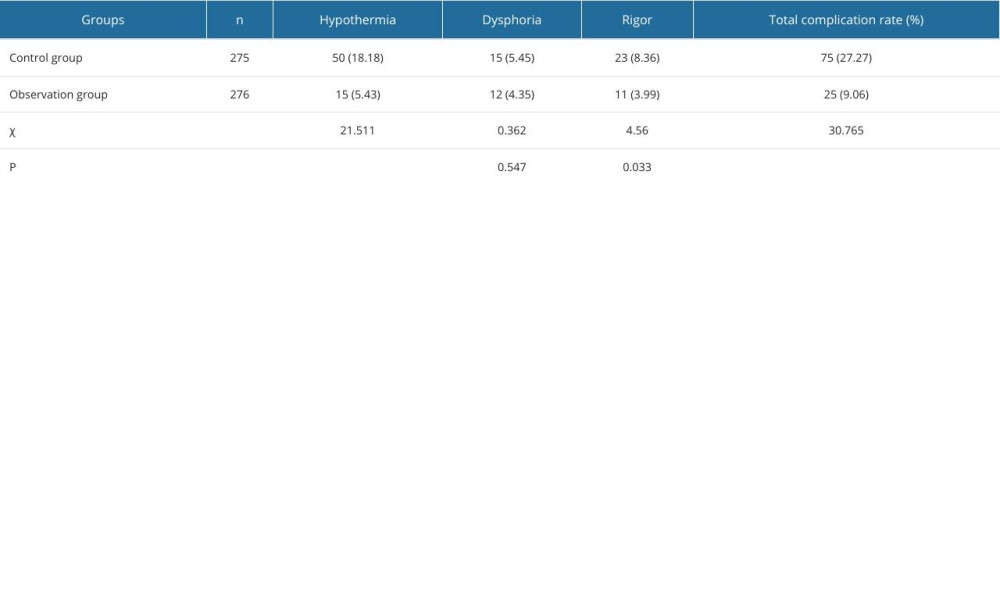 Table 5. Complications in the 2 groups [n (%)].
Table 5. Complications in the 2 groups [n (%)]. In Press
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952