26 March 2024: Clinical Research
A Retrospective Study of the Presentation and Management of Perianal Disease in HIV-Positive Patients Referred to a Surgical Outpatient Unit in Turkey
Omer Faruk BukDOI: 10.12659/MSM.943534
Med Sci Monit 2024; 30:e943534
Abstract
BACKGROUND: The incidence of human immunodeficiency virus (HIV) infection is on the rise, and perianal region diseases in HIV-infected patients have become increasingly prevalent. This study aimed to analyze the surgical treatment outcomes of HIV-infected patients presenting with perianal concerns.
MATERIAL AND METHODS: We included 311 HIV-positive patients admitted to the Infectious Diseases Clinic of Samsun Training and Research Hospital between January 2014 and December 2022. From this group, we selected those who sought care at the general surgery outpatient clinic for perianal and anal concerns, retrospectively reviewing their medical records.
RESULTS: Out of 311 patients, 54 (17.3%) were referred to the general surgery outpatient clinic with anal and/or perianal region complaints. Of these cases, 38 (70.3%) had a single disease, while 16 (29.6%) had combined diseases. There were 20 males (95%) and 1 female (5%). Among these 54 patients, 33 (61.1%) received medical treatment from the outpatient clinic, while 21 (38.9%) underwent surgical intervention. The diagnoses included 22 hemorrhoidal diseases, 24 anal condylomas, 15 anal fissures, 11 anal abscesses, and 4 anal fistulas. We evaluated the postoperative results and recurrence status of these patients.
CONCLUSIONS: Perianal diseases in HIV-positive patients can be categorized as isolated or combined. The management of patients with postoperative follow-up compliance problems and combined diseases with low CD4 counts may pose treatment challenges.
Keywords: Acquired Immunodeficiency Syndrome, Condylomata Acuminata, HIV, Wound Healing, Anus Diseases
Introduction
Human immunodeficiency virus (HIV) infection is a systemic disease that can manifest with systemic involvement in various organs, including the esophagus, stomach, small bowel, colon, and perianal region [1], present ing with symptoms such as diarrhea, vomiting, abdominal pain, and perianal discomfort. Studies have indicated that perianal problems are the initial signs of HIV infection in a subset of patients [2]. While anorectal abscesses and fistulas are relatively uncommon pathologies in the general population, they are more prevalent in individuals with HIV infection [3]. In fact, anorectal pathologies are detected in approximately one-third of HIV-positive patients, with half of them eventually requiring surgical intervention [4]. Patients with HIV infection can develop both common and unique anorectal problems [5]. Anorectal diseases in HIV patients can occur in 3 ways: (1) HIV-related anal ulcers as an HIV-associated anorectal condition; (2) manifesting as a disease, such as anal condyloma, which occurs with HIV infection and behaves differently from its normal course; (3) hemorrhoidal disease or condition in patients with or without HIV infection of all age groups [6]. Perianal pathologies in HIV-positive patients can be benign or malignant, with benign lesions being more common and often localized in the perianal region. Malignant lesions, such as squamous cell carcinoma of the anus and cutaneous Kaposi sarcoma, can also occur in HIV-positive patients, contributing to the heterogeneity of clinical presentations in this population [7]. Male patients infected with HIV can present with anorectal diseases that include hemorrhoids, anal ulcers, condylomas (warts), anal fissures and fistula, and perianal and perirectal abscesses. Surgical procedures and treatments for anorectal diseases in patients with HIV include perianal abscess drainage, seton placement, excisions for anal condylomas, and hemorrhoidectomy [8]. Therefore, this retrospective study describes the presentation and management of perianal disease in HIV-positive patients referred to a surgical outpatient unit in Turkey between 2014 and 2022.
Material and Methods
ETHICS STATEMENT:
All procedures involving human participants were conducted in accordance with ethical standards as outlined in the 1964 Helsinki Declaration and its later amendments. Ethics approval was granted by the Institutional Review Board of Samsun Training and Research Hospital (Institutional Review Board No. SUKAEK-2022-10/9). Written informed consent was obtained from the patients for publication of images.
STUDY DESIGN AND PATIENTS:
We enrolled 311 HIV-positive patients who sought care at Samsun Training and Research Hospital’s Infectious Diseases Clinic between January 2014 and December 2022 and were subsequently referred to the general surgery clinic due to anal or perianal complaints. We retrospectively evaluated patient demographics, diagnoses, surgical procedures performed, postoperative outcomes, and complications. We gathered data on patients with anal and perianal diseases from hospital records and files, supplemented by follow-up information obtained through telephone interviews. Patients admitted to the outpatient clinic underwent further evaluation and examination.
STATISTICAL ANALYSIS:
Statistical analysis was conducted using SPSS 25.0 (SPSS, Inc., Chicago, IL). Data are presented as means with standard deviations.
Results
We reviewed the records of 311 HIV-positive patients who attended the Infectious Diseases Clinic of Samsun Training and Research Hospital between January 2014 and December 2022. Of these, 54 patients (17.3%) were referred to the general surgery outpatient clinic for anal and/or perianal region concerns. Among the 54 patients, 33 (61.1%) received medical treatment from the outpatient clinic, while 21 (38.9%) underwent surgical intervention. There were 20 male patients (95%) and 1 female patient (5%). The median age at presentation was 36 years (range: 23–67 years), with an average symptom duration of 22.8 months (range: 12–48 months) before seeking medical attention. Initial symptoms varied, including perianal mass (28.6%), perianal swelling and discharge (19%), perianal swelling and bleeding (19%), and other combinations. Single diseases were detected in 38 patients (70.3%), while 16 patients (29.7%) had combined diseases. Among patients with single diseases, the most common conditions were anal condyloma (29.6%), anal fissures (9.2%), and perianal abscesses (7.2%). In the group with combined diseases, various combinations were observed, with the most frequent being hemorrhoids and anal fissure (7.2%), hemorrhoids, anal fissure, and anal abscess (5.5%), anal condyloma and anal fistula (3.7%), and perianal abscess, anal fistula, and anal condyloma (3.7%). The total number of diagnoses included 22 hemorrhoidal diseases, 24 anal condylomas, 15 anal fissures, 11 anal abscesses, and 4 anal fistulas. A schematic representation of the patients is presented in Table 1.
Among the 21 patients who underwent surgical intervention, 7 (33.3%) received inpatient surgical treatment, while 14 (66.7%) received outpatient surgical treatment. Procedures performed on hospitalized patients included perianal abscess drainage (11 cases), seton placement (2 cases), electrocautery excisions for anal condylomas (9 cases), hemorrhoidectomy (1 case), and condyloma excisions (3 cases). Regional anesthesia was administered to 7 inpatients (33.3%), while local anesthesia was administered to the remaining 14 patients (66.7%). The mean postoperative hospital stay was 1.28 days, and the postoperative course was uneventful, except for seton revision in one patient and cauterization repeat for anal condyloma in another. Patient demographics, surgical outcomes, and outpatient clinic follow-ups at 6 and 12 months are summarized in Table 2. Figure 1 shows a photographic image of a perianal fistula in an HIV-positive patient.
Discussion
This study aimed to contribute to the existing literature by examining the surgical treatment outcomes of perianal diseases in HIV-positive patients. Previous studies have shown that one-third of HIV-positive individuals develop anorectal pathology, with approximately half requiring surgical intervention [1,4,9]. In our study, 54 patients (17.3%) out of 311 HIV-positive individuals presented with perianal concerns, and 21 (38.8%) of them underwent surgical treatment, while others received medical treatment. Anal condyloma was the most common diagnosis in both groups, followed by hemorrhoids, anal fissures, perianal abscesses, and anal fistulas. Unlike some studies reporting ulcerated lesions or malignancies in HIV-positive patients, our study did not identify any such cases [3,10].
In the context of combined anal diseases in HIV-positive patients, the rate has been reported to range from 16% to 66%, aligning with our finding of 29.6% [2,3]. Perianal problems are the initial symptoms of HIV infection in some cases, highlighting the importance of considering HIV infection in patients presenting with multiple anal diseases [2]. Remarkably, a significant portion of patients in our study (28.6%) were unaware of their HIV-positive status until the pre-operative work-up, emphasizing the importance of routine serological tests in patients with perianal problems.
Previous studies have reported varying rates of disease recurrence [11,12]. Our study found recurrence rates of 42.9% and 47.6% for condyloma acuminata at 6 and 12 months, 28% and 19% for hemorrhoids, 28% for anal fissures, and 47% and 52.4% for anal fistulas, and 14% and 23.8% for abscesses, respectively. These higher recurrence rates in some conditions may be attributed to combined disease presentations and patients’ failure to return for regular follow-ups.
The CD4/CD8 ratio, an indicator of immune status, was considered in our study since we could not obtain CD4 measurements. A low CD4/CD8 ratio has been associated with impaired wound healing in HIV-positive patients, potentially contributing to higher recurrence rates in our study [13,14].
This study had several limitations. First, it had a retrospective design and was conducted in a single center. Second, the management of perianal disease in HIV-infected patients and its relationship with CD4 count and immunologic status and its effect on clinical parameters with long-term follow-up was not fully evaluated. Finally, the number of patients was small.
Conclusions
HIV infection is a multifaceted condition, and perianal diseases in HIV-positive patients can present as isolated or combined pathologies. Anal condylomas are the most prevalent lesions encountered in surgical clinics among HIV-positive patients. The stage of the disease, CD4 counts, presentation type, follow-up, and patient compliance with treatment are crucial factors affecting treatment success. In managing these patients, special consideration should be given to those with postoperative follow-up compliance problems and those presenting with combined diseases, which may exhibit increased resistance to treatment.
References
1. Edwards P, Wodak A, Cooper DA, The gastrointestinal manifestations of AIDS: Aust N Z J Med, 1990; 20(2); 141-48
2. Barrett WL, Callahan TD, Orkin BA, Perianal manifestations of human immunodeficiency virus infection: Experience with 260 patients: Dis Colon Rectum, 1998; 41(5); 606-11 discussion 611–12
3. Nadal SR, Manzione CR, Galvao VM, Perianal diseases in HIV-positive patients compared with a seronegative population: Dis Colon Rectum, 1999; 42(5); 649-54
4. Wexner SD, Smithy WB, Milsom JW, Dailey TH, The surgical management of anorectal diseases in AIDS and pre-AIDS patients: Dis Colon Rectum, 1986; 29(11); 719-23
5. Yuhan R, Orsay C, DelPino A, Anorectal disease in HIV-infected patients: Dis Colon Rectum, 1998; 41(11); 1367-70
6. Weiss EG, Wexner SD, Surgery for anal lesions in HIV-infected patients: Ann Med, 1995; 27(4); 467-75
7. Schulberg S, Al-Feghali V, Bain K, Shehebar J, Non-cutaneous AIDS-associated Kaposi’s sarcoma presenting as recurrent rectal abscesses: BMJ Case Rep, 2018; 2018; bcr2018225749
8. Geminiano-Martinez EE, Ruiz-Esparza JP, Villanueva-Saenz EAnorectal surgery in patients infected with human immunodeficiency virus: Rev Gastroenterol Mex, 2000; 65(4); 152-58 [in Spanish]
9. Safavi A, Gottesman L, Dailey TH, Anorectal surgery in the HIV+ patient: Update: Dis Colon Rectum, 1991; 34(4); 299-304
10. Consten EC, Slors FJ, Noten HJ, Anorectal surgery in human immunodeficiency virus-infected patients. Clinical outcome in relation to immune status: Dis Colon Rectum, 1995; 38(11); 1169-75
11. Manzione CR, Nadal SR, Calore EE, Postoperative follow-up of anal condylomata acuminata in HIV-positive patients: Dis Colon Rectum, 2003; 46(10); 1358-65
12. Oh HK, Moon SH, Ryoo S, Results of surgical treatment on benign anal diseases in Korean HIV-positive patients: J Korean Med Sci, 2014; 29(9); 1260-65
13. Castilho JL, Bian A, Jenkins CA, CD4/CD8 ratio and cancer risk among adults with HIV: J Natl Cancer Inst, 2022; 114(6); 854-62
14. Lord RV, Anorectal surgery in patients infected with human immunodeficiency virus: Factors associated with delayed wound healing: Ann Surg, 1997; 226(1); 92-99
Tables
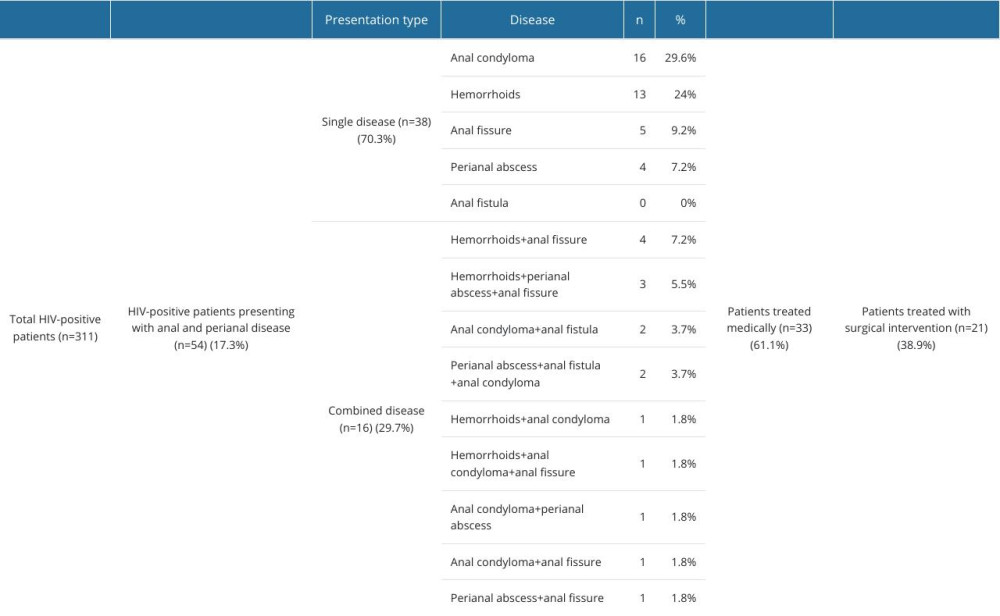 Table 1. A schematic presentation of patients included in the study.
Table 1. A schematic presentation of patients included in the study.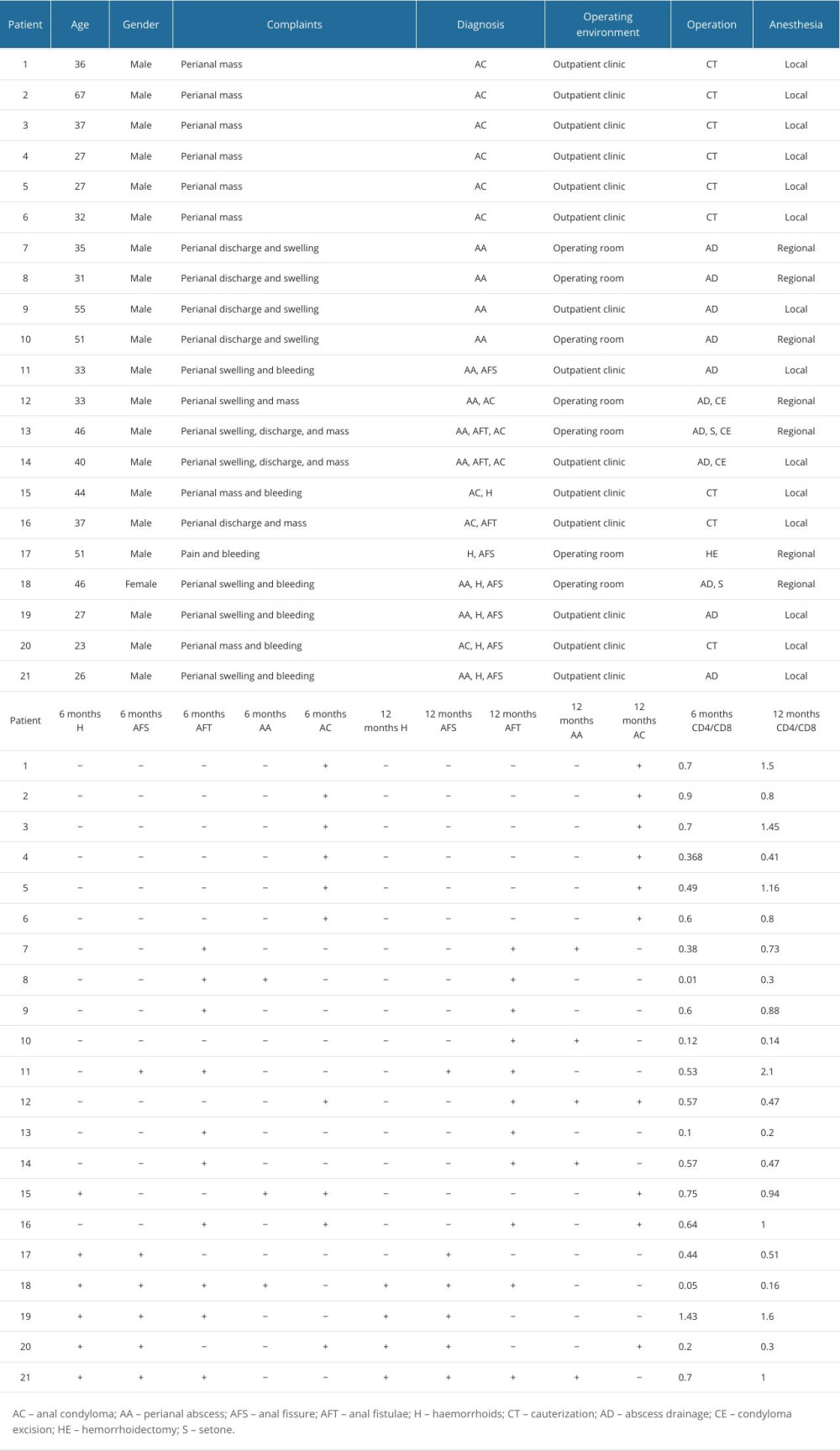 Table 2. Demographics, surgical outcomes, and outpatient clinic follow-up of patients.
Table 2. Demographics, surgical outcomes, and outpatient clinic follow-up of patients.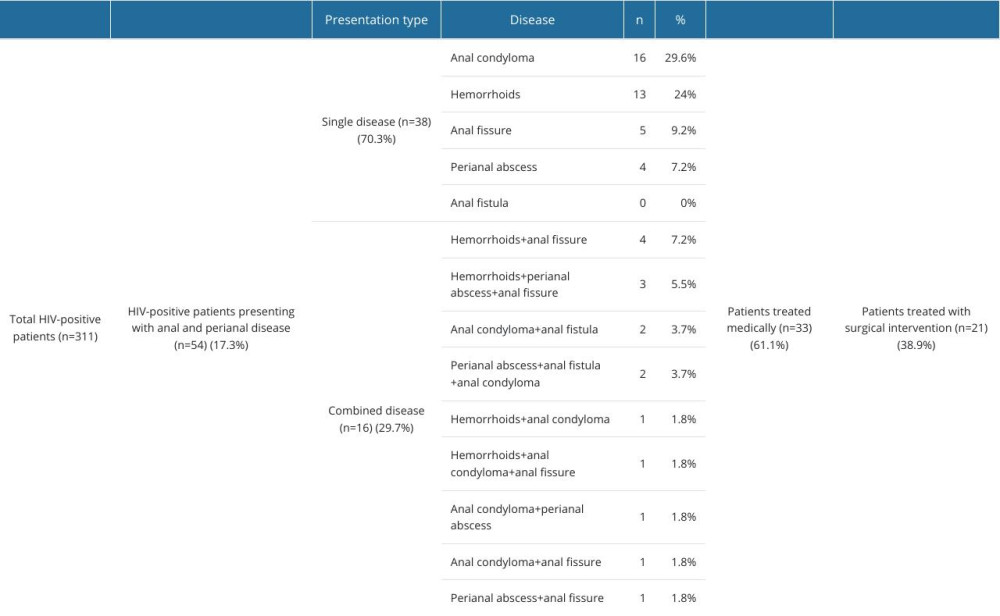 Table 1. A schematic presentation of patients included in the study.
Table 1. A schematic presentation of patients included in the study.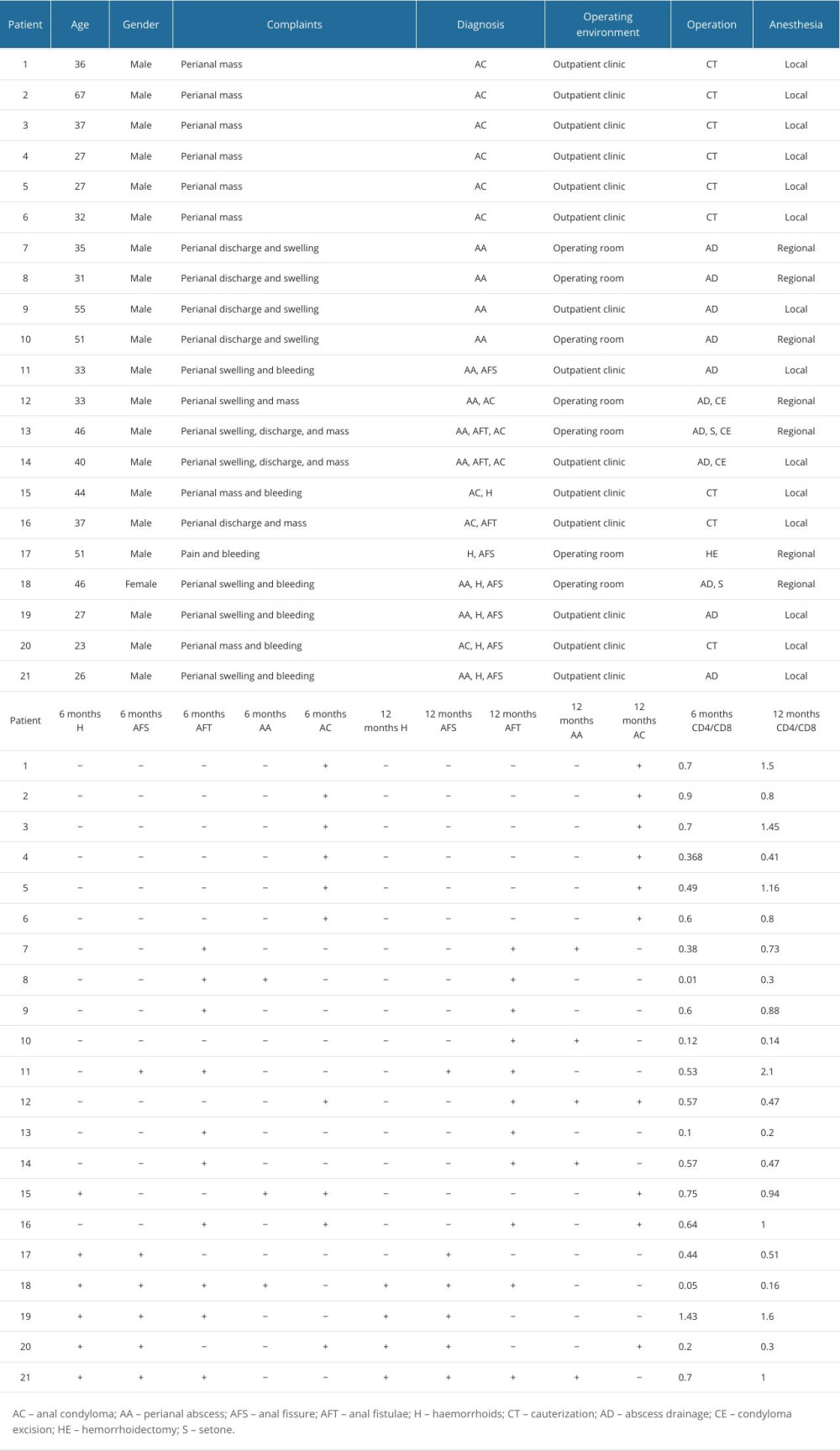 Table 2. Demographics, surgical outcomes, and outpatient clinic follow-up of patients.
Table 2. Demographics, surgical outcomes, and outpatient clinic follow-up of patients. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









