25 April 2024: Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body Mass
Aleksandra Kopaczyńska1BCEF, Alicja Bober1BCE, Agnieszka Puk1BCE, Agnieszka ChwałczyńskaDOI: 10.12659/MSM.943765
Med Sci Monit 2024; 30:e943765
Abstract
BACKGROUND: The human foot has a complex structure and the ligamentous and muscular apparatus undergoes transformation and adaptation during its ontogenetic development. Excessive body mass may be one of the factors disrupting proper foot formation. This study aimed to assess the foot structure in preschool children in relation to body mass.
MATERIAL AND METHODS: A total of 105 children aged 6.27±0.60 years were examined. Height, weight, and segmental body composition were determined using the Tanita MC-780 body composition analyzer. The foot structure was assessed using the Kasperczyk method, supplemented with digital analysis using the Podoscan 2D camera. The Weisflog index and gamma angle for feet were calculated. Children were divided into 2 groups: children in Group I did not have foot deformities and those in Group II had foot deformities.
RESULTS: No correlation was observed between body mass and the occurrence of anomalies in foot structure. A correlation was noted between the Weisflog index for the right foot and height in both groups. The Weisflog index for both feet was correlated with BMI, with higher values obtained for the left foot in both groups. In Group II, a correlation was observed between the gamma angle value for the left foot and the predicted muscle mass for the right lower limb, as well as between the same foot and the predicted muscle mass for the left lower limb.
CONCLUSIONS: No correlation was observed between high BMI and the occurrence of anomalies in foot structure. A relationship was identified between muscle mass and foot structure.
Keywords: Foot Deformities, Pediatric Obesity
Introduction
The human foot is a crucial static-dynamic component of the musculoskeletal system that throughout phylogenetic evolution has undergone numerous adaptations to facilitate the bearing of substantial and dynamic loads. A properly structured foot comprises 26 bones forming 33 joints interconnected by numerous ligaments. It is divided into 3 segments: the posterior (hindfoot), middle (midfoot), and anterior (forefoot). Additionally, the foot skeleton has medial and lateral longitudinal arches, as well as a transverse arch, crucial for providing resilience and flexibility to the foot while absorbing shocks and microtrauma during locomotion. To fulfill their functions without losing elasticity and resilience, these arches must be supported by strong ligaments, tendons, and muscles [1–5].
The shape and structure of a child’s foot immediately after birth are primarily determined by soft tissues. A child is born with flat feet. However, significant transformations rapidly occur within the musculoskeletal system as cartilaginous tissue ossifies, adapting to bear increasing loads. During this period, the presence of a fat pad is normal just beneath the medial longitudinal arch, protecting against overloading until the foot architecture develops correctly. The most advanced morphological and physiological development of the feet is noticeable up to the age of 3 years, continuing until achieving a foot structure similar to that of an adult by around 5 or 6 years old. This is attributed to the intense development during the preschool period, associated with a high degree of freedom of movement, leading to increased strength in the muscle-ligament system of the feet. During these ongoing physiological changes, children have flat feet until around the age of 5 years. A properly arched foot is typically observed in children around the age of 9 years when the structures of all foot arches mature and stabilize [1,2,5,6].
The human foot serves 2 fundamental roles in the human body. The first is its dynamic function, involving movement and adaptation to changes in terrain, loads, and positions. The second is its static function, providing support for maintaining an upright posture. Ultimately, any deviations from the norm in foot structure are reflected in the pathogenesis of disorders in other parts of the musculoskeletal system [4,5].
Among the most common abnormalities in foot structure are flatfoot, flatfoot-valgus, cavus foot, and equinovarus foot. Flatfoot is characterized by weakened ligaments and muscles that support the foot structure, leading to a lowering of the longitudinal arches, causing the entire plantar surface to contact the ground. In the case of flatfoot-valgus, in addition to the changes described above, there is also a pronated positioning of the heel bone. In the case of a cavus foot, a high positioning of the medial longitudinal arch is observed, with the heel bone typically being more inverted. Equinovarus foot is characterized by a lowering of the lateral edge of the foot, forefoot adduction, and elevation of the heel bone above the ground. Epidemiological and anthropometric factors can stimulate or contribute to development of these deformities. These factors include age, as it is a primary predictive factor for flatfoot, and the frequency of flatfoot decreases gradually with age. Additionally, a significant contributing factor is overweight and obesity in children, which increases the frequency of flatfoot compared to children with normal body weight [5–12].
The results of epidemiological studies reveal a continuous upward trend in the occurrence of high body mass index (BMI) in humans. The most concerning observation is the increasingly common diagnosis of overweight and obesity in progressively younger age groups. The highest risk of an elevated BMI occurs during critical periods in the development of children and adolescents when the number of fat cells in the body increases. These critical periods correspond to the first and second years of life, the fifth and seventh years of life, and puberty [13]. According to the International Obesity Taskforce, childhood obesity is a serious health crisis with numerous long-term consequences related to the cardiovascular system, development of diabetes, and psychosocial disturbances [14]. Research also indicates numerous musculoskeletal deformities associated with high BMI. Obesity may result from reduced physical activity despite adequate energy intake, leading to joint overload, especially in the lower limbs and spine. In the lower limbs, the most common outcome is development of flat feet due to overloading the foot arches. Structural changes are associated with discomfort and pain, potentially limiting the child’s activity and mobility [13,15,16].
The study aimed to assess the frequency and nature of foot structure abnormalities in preschool-aged children based on their BMI. Additionally, a segmental body composition assessment was introduced to determine the symmetry of fat and lean tissue distribution in preschool-aged children and to identify their relationships with the occurrence of foot abnormalities.
Material and Methods
Approval for the study was obtained from our local bioethics committee. The research complied with the Helsinki Declaration, and we obtained written informed consent from parents/legal guardians and verbal consent from the children to conduct the study.
In the study, 105 children participated (46% females) with an average age of 6.27±0.60 years (females: 6.29±0.62 years, males: 6.24±0.58 years) from a preschool. The mean body weight of the children was 21.9±3.5 kg (females: 22.1±3.8 kg, males: 21.8±3.2 kg), and the mean height was 117.5±5.8 cm (females: 117.2±5.2 cm, males: 117.7±6.3 cm). No statistically significant differences were observed between the studied groups.
The conditions for inclusion in the study group were: obtaining the consent of the parent/legal guardian to participate in the research project, the child’s consent to participate in the study, no contraindications to the use of the bioelectrical impedance method (pacemaker, metal elements in the body, active neoplastic disease), posture defects diagnosed by a doctor, foot defects, wearing orthopedic shoes for medical reasons, and participating in physiotherapy classes to correct posture defects.
Height was measured with an accuracy of 0.1 cm using the SECA 213 stadiometer, and body weight and composition were determined using the Tanita MC-780 eight-electrode body composition analyzer (Tanita Company, Japan), which uses the innovative multi-frequency technology using the bioelectrical impedance method (BIA), with GMON Health Monitor software. The device is approved for medical use covered by directive 93/42/EEC (MDD) or the new regulation 2017/745 (MDR). Measurements were conducted in the morning, and the children participated in the study wearing sportswear (shorts) and barefoot. Total and segmental fat mass (FM% and FM [kg]), lean mass (FFM [kg]), and predicted muscle mass (PMM [kg]) were determined. Body mass index (BMI [kg/m2]) was calculated based on body weight and height. To assess deviations in body weight, the BMI centile value for age and gender was utilized, employing BMI centile charts from the OLAF and OLA software (2010) [17,18]. The WHO classification was used, dividing body weight according to BMI values as underweight (BMI <5th centile), normal body weight (5< BMI <85th centile), and overweight (BMI >85th centile). A separate group for obesity (BMI >95th centile) was not distinguished.
The subjects were divided into 2 groups based on the presence of foot structure abnormalities assessed through physiotherapeutic evaluation, following the diagnostic standards according to Kasperczyk. Foot abnormalities included flat feet (flattening of the longitudinal arch), flat-valgus feet (flattening of both the longitudinal and transverse arches), cavus feet (deepening of the arch between the heel and the heads of the metatarsal bones with a simultaneous shortening of this section), and equinovarus feet (inward rotation of the heel with simultaneous contact on the outer edge) [19,20]. Group I (N=50; including 50% girls) consisted of children without foot structure abnormalities and Group II (N=55; including 43.6% girls) consisted of children with foot structure abnormalities. Physiotherapeutic examinations were conducted to assess for foot abnormalities, specifying the side affected—right, left, or both. In Group I, the most common foot abnormality was flat-valgus feet on the right and left (58%) and flat feet on the right and left (29%), with no occurrences of equinovarus or cavus feet.
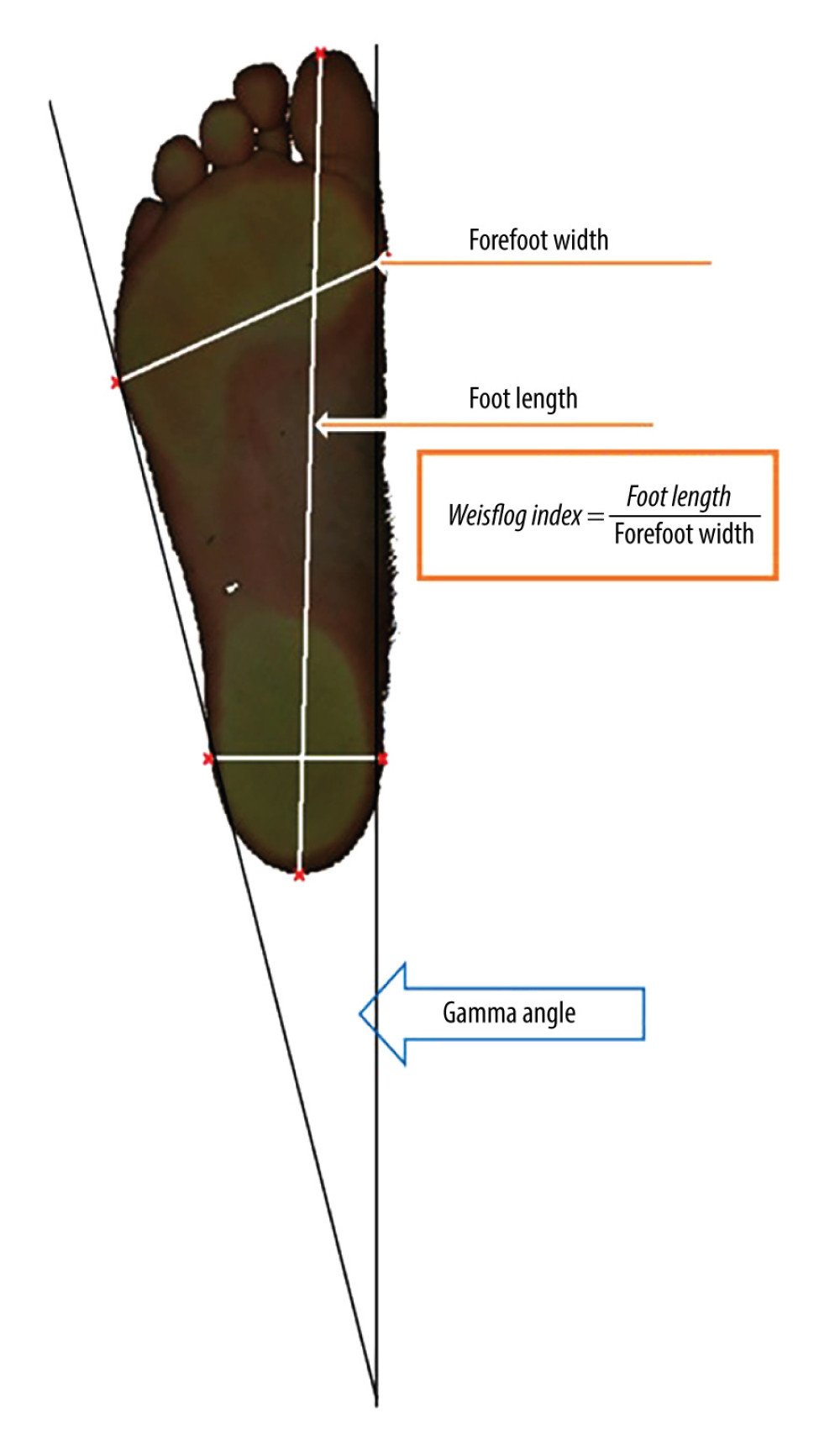
The visual physiotherapeutic assessment was supported by a digital analysis of footprints and plantar pressures using the Podoscan 2D FreeSTEP-V.1.4.01 SENSOR MEDICA apparatus, conducted on all participants. The Podoscan 2D camera uses a CCD guide with a cold cathode (1600 DPI), ensuring very high sensitivity and resolution of the obtained plantocontourogram image, along with the observation of supporting spheres, providing a three-dimensional image of the shape of the arch of the foot. The examination took place while standing barefoot. Based on the obtained analysis, the length and width, Weisflog index, and gamma heel angle were determined for the right and left foot. The Wejsflog index is calculated based on the length and width of the foot and is used to assess the longitudinal arch of the foot. The length of the foot is measured from the end of the toe to the end of the heel. The width of the foot is determined at the widest point of the forefoot from the outer to the inner line. The gamma angle, also called the heel angle, is determined by 2 inner and outer tangents that create an angle beyond the heel (Figure 1). The gamma angle is used to assess the position of the foot in a valgus or varus position. Segmental body composition analysis was performed, focusing on the right and left lower limbs. Under normal conditions, the Weisflog index should be 2.55–3.00, representing the ratio of foot length to width, indicating proper arching of the foot. Values below 2.55 indicate the presence of transverse flatfoot [21,22]. Normative values for the gamma heel angle of the foot should be 15°–18°. Values below 15° indicate valgus foot alignment, while values above 18° suggest varus foot alignment [22,23].
The obtained results were analyzed using the Statistica 13.3 software package. Descriptive statistics, mean, and standard deviation (SD) were used to describe the groups. The Shapiro-Wilk test was applied to assess the normality of the distribution for the examined variables within the groups. Non-parametric statistics for independent groups, including the Mann-Whitney U test, were employed for between-group comparisons. Parametric statistics for independent groups and the chi-square test were utilized for comparisons. Correlation was determined using Spearman’s rank correlation. The statistical significance level was set at
Results
Statistically significant differences were observed in the height and body weight of the examined children depending on the presence of foot structure abnormalities. Participants in Group I had higher BMI, a greater amount of fat tissue, and higher predicted muscle mass. Detailed results are presented in Table 1.
Over 85% (Group I – 88%, Group II – 85.5%) of the examined children were within the weight norm for their age and gender. In 10% of participants from Group I and 9% from Group II, a BMI below the 5th centile was observed, indicating underweight. No statistically significant differences (chi-square=0.279) were found in the distribution of body weight norms based on the presence of foot structure abnormalities.
The mean values of the Weisflog index for left and right feet were 2.55–3.00, indicating proper arching. In Group I, a statistically significant difference was noted between the right and left sides. The obtained values for the heel angle for left and right feet in both groups were decreased, indicating valgus foot alignment. No statistically significant differences were found in gamma angle values between the right and left sides or between Groups I and II (Table 2).
Analyzing the correlations, we observe that most of the obtained data had very weak relationships. However, in Group I, there was a weak positive correlation between the Weisflog index for the right foot and body height. There was a weak negative correlation between the Weisflog index for the left foot and BMI, greater for the left foot. In Group II, a weak positive correlation was noted between the Weisflog index for the right foot and body height, as well as between the gamma heel angle for the left foot and BMI. Similar to Group I, the Weisflog index for right and left feet was weakly negatively correlated with BMI, but, as in Group I, higher values were obtained for the left foot. The results are presented in Table 3.
The relationships between the Weisflog index and the gamma heel angle for the right and left feet and the level of fat and predicted muscle mass in Group I showed a very weak correlation, as presented in Table 4. In Group II, the gamma heel angle for the left foot and RL PMM exhibited a weak positive correlation. Similarly, a correlation was observed between the gamma heel angle of the same foot and LL PMM. The remaining relationships in Group II were very weak.
Discussion
Since the early 2000s, there has been a noticeable increase in research on the topic of overweight and obesity in children and their impact on posture and foot structure, showing that children with normal body weight or underweight and children with above-normal body weight experience problems with abnormalities in foot structure. These abnormalities were associated with the occurrence of flat feet [6,24]. Foot defects affected more than half of the examined children. In obese children, no abnormalities in foot structure were observed, but this may be because only 2 children were classified as obese. According to the research, there were no statistically significant differences in the number of children with abnormal body weight between the groups.
Attention should be drawn to the fact that in the presented studies, a correlation appeared between the Weisflog index, height, and BMI. The values of the Weisflog index for the right feet in both groups fell within the norms for a properly formed transverse arch and were associated with greater height. The opposite relationship was observed concerning the Weisflog index and BMI – the closer the Weisflog index was to 3.00, the lower the child’s BMI.
According to studies by other authors, analyzing various parameters to assess foot structure can determine the most common foot abnormalities and their severity. Mickle et al found a correlation between high BMI and more frequent occurrences of flat feet in children. Their research suggests that not only obesity but also overweight leads to increased contact of the midfoot with the ground [2]. The difference between the results of these studies and those presented in the present study may be related to the age of the children. In Mickle et al’s study, the examined children were on average 2 years younger, and their group was smaller. The feet of children at age 4 years are more flexible due to a weaker muscle-ligament system than at the age of 6, when the foot already has the characteristics of an adult foot. In the group examined by Mickle et al, the physiological arch of the foot tended to be lower, associated with ontogenetic changes in foot structure and walking mechanics at this age [1,6]. Similar results were obtained in a group of preschool children by Walicka-Curpryś et al [22]. Pauk et al found an increased risk of flat feet in children with above-normal body weight due to their less active lifestyle [24]. Discrepancies between the findings of Pauk et al again focused on the age of the examined children. The group was examined at the age of 7–15 years, and it was much larger than in our study [24]. Wacławek et al, after performing a statistical analysis of the obtained data, demonstrated a correlation between the gamma angle of the left foot in 4- and 5-year-old children, where a higher index was noted for the 4-year-olds [5]. However, in these studies, no comparison was made between the obtained data and body weight, and the group was smaller than in our study.
The children we examined were at an age when the occurrence of flat feet is still considered physiological. Similar conclusions were drawn by Mikołajczyk and Jankowicz-Szymańska, noting that specific abnormalities in foot and lower limb structure are common in 7-year-olds [25]. Chang et al, who examined school-age children, observed that flat feet were more common at age 7 and 8 years than in later years, confirming that it can occur at this age and is not immediately considered to be pathological [26].
Some authors also point out other factors that may be equally strongly associated with the development of flat feet as obesity. Mickie et al found that the risk of flat feet increases with age [2]. Makarczuk et al assessed the influence of the environment in which a child is raised, including the awareness of parents and caregivers about risk factors for development of posture defects and foot structure abnormalities, finding that education in prevention of posture defects is necessary for parents and educators [27].
Our research also assessed segmental body composition, showing that normal foot structure was associated with less body fat and more muscle tissue in the lower limbs. A statistically significant but weak correlation was observed between the gamma heel angle and distribution of muscles and fat in both lower limbs. The larger the recorded gamma heel angle, the more developed the muscles of the examined limb were, and consequently, the foot structure was more likely to be normal. Ziętek et al showed the importance of using segmental body composition analysis as a screening method for posture defects, and that muscle mass and percentage of body fat play a crucial role in development of correct body posture in young school-age children [28].
Ziętek et al demonstrated that the balance between muscle mass and the percentage of body fat plays a crucial role in shaping correct body posture, including proper foot structure [28]. Increased fat mass around the foot in preschool-age children indicates the presence of a fat pad typical for this age. Riddiford-Harland et al suggested that this fat pad serves a cushioning function when transferring greater weights in children with above-average BMI, thus protecting the musculoskeletal system [28,29]. Studies indicate that the resorption of the fat pad begins with the onset of independent walking, but the precise time of its disappearance is unclear [1]. Muscle development in the foot-shaping process leads to a greater contribution of muscle mass compared to body fat, resulting in remodeling of the foot. Well-developed foot muscles ensure proper construction of the arch and contribute to the foot’s proper functioning [14].
Many authors who studied the relationship between body weight and foot structure abnormalities remarked on the insufficient recognition of this topic and the need to study different age groups [28–32].
Conclusions
In summary of the collected results from our research and observations from studies by other authors, it is noted that flat feet in preschool-age children are a physiological phenomenon and not necessarily linked to overweight or obesity. The existence of a relationship between the amount of muscle mass and a higher gamma heel angle may indicate that insufficient muscle mass predisposes to the occurrence of abnormalities in foot structure. These conclusions should be confirmed by conducting studies on a much larger scale.
Tables
Table 1. Comparison of anthropometric values between the studied groups based on the presence of foot structure abnormalities.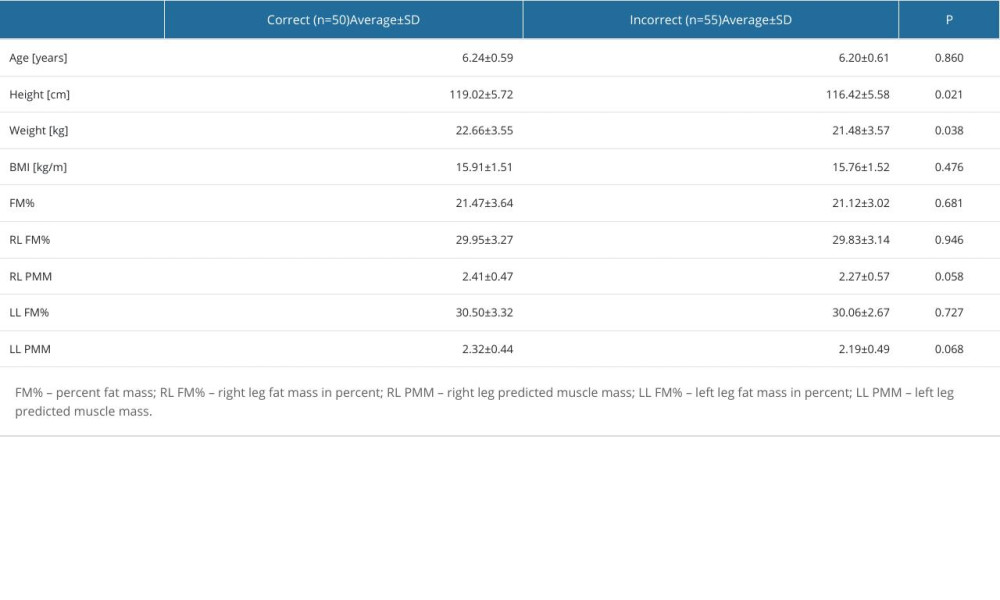 Table 2. Results of calculated Weisflog index and gamma angle.
Table 2. Results of calculated Weisflog index and gamma angle.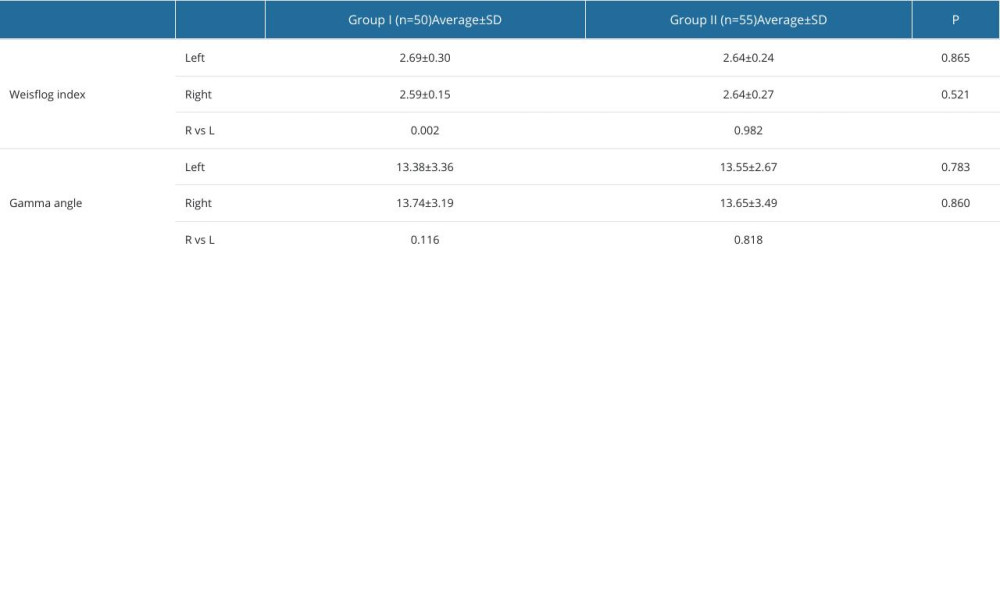 Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.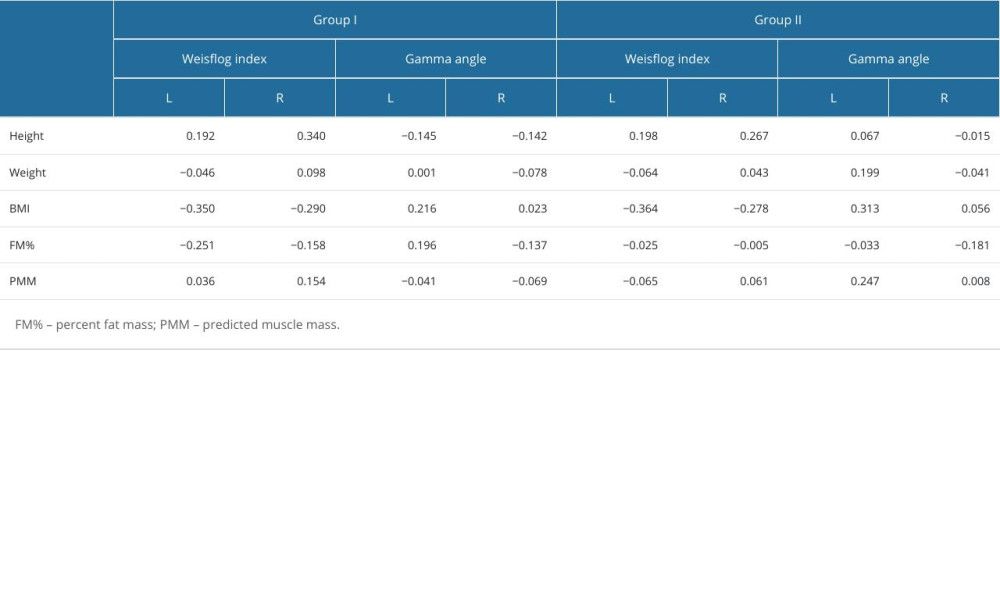 Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.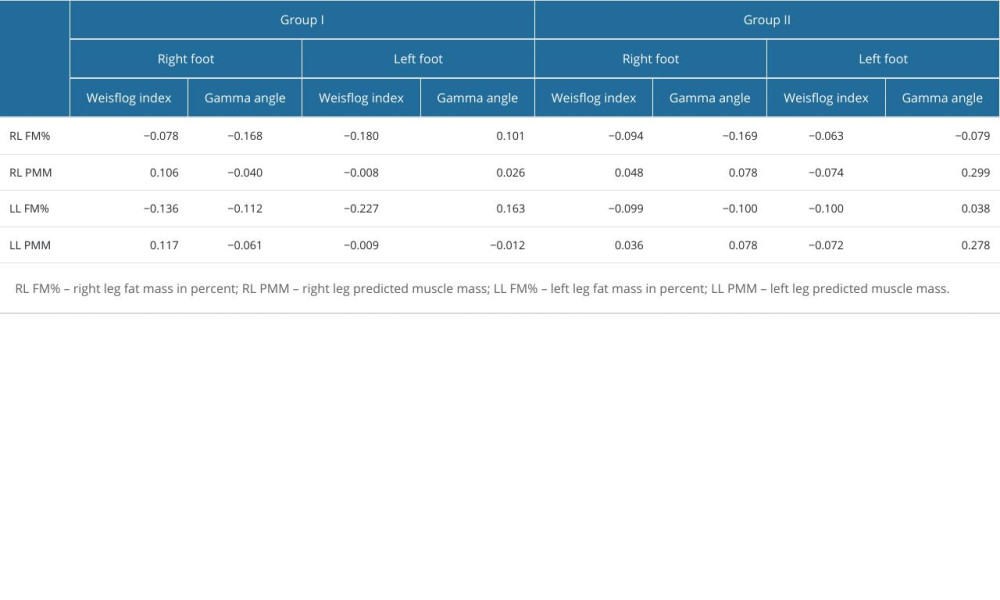
References
1. Mickle KJ, Steele JR, Munro BJ, Is the foot structure of preschool children moderated by gender?: J Pediatr Orthop, 2008; 28(5); 593-96
2. Mickle KJ, Steele JR, Munro BJ, The feet of overweight and obese young children: Are they flat or fat?: Obesity, 2006; 14(11); 1949-53
3. Bochenek A, Reicher M: Human anatomy. Volume I, 2021; 518–616; 852-933, Warsaw, Medical Publishing House PZWL
4. Furgał W, Adamczyk A, The shape of the foot arch in children depending on body mass index: Sports Medicine, 2009; 3(6); 189-99
5. Wacławek P, Drzał-Grabiec J, Truszczyńska A, Foot development in preschool children: Rehabilitation Progress, 2015; 1; 13-20
6. Villarroya MA, Esquivel JM, Concepcion T, Foot structure in overweight and obese children: I J Pediatr Obes, 2008; 3; 39-45
7. Pfeiffer M, Kotz R, Ledl T, Prevalence of flat foot in preschool-aged children: Pediatrics, 2006; 118(2); 634-39
8. Ignasiak Z: Anatomy of the movement system, 2007; I, Wrocław, Elsevier Urban & Partner
9. Szubski D, Czachor M, Digital Database for diagnostic tests of foot deformities in children and adolescents: Current Problems of Biomechanics, 2010; 4; 201-6
10. Misztal-Okońska P, Okoński P, Goniewicz MThe history of treatment of congenital club footj: Archiwum Historii i Filozofii Medycyny, 2016; 79; 32-36 [in Polish]
11. Okoński M, Misztal-Okońska P, Kandzierski G, Changes in the focus of clinical paediatric orthopaedics in the period 1980–2021 on the example of the Department of Children’s Orthopaedics and Rehabilitation in Lublin: Chir Orthop Movement Organs Half, 2021; 86(2); 50-58
12. Pardus K, Stencel-Gabriel K, Kurdyś P, Analysis of selected methods of diagnostics and physiotherapy of pes plano-valgus in children: Journal of Education, Health and Sport, 2022; 12(11); 18-22
13. Srokowska A, Piernicka D, Lewandowski A, Weight and flat feet in children of preschool age – research report: Journal of Education, Health and Sport, 2015; 5(4); 380-404
14. International Obesity Task Force and European Association for the Study of Obesity: Obesity in Europe: The case for sction, 2002, London, International Obesity Taskforce
15. Morrison SC, Durward BR, Watt GF, Anthropometric foot structure of peripubescent children with excessive versus normal body mass. A cross-sectional study: J Am Podiatr Med Associ, 2007; 97(5); 366-70
16. Przysada G, Luszowska A, Drużbicki M, Defects of feet at children with intellectual incompetence: Young Sport Science of Ukraine, 2010; 3; 163-68
17. Kułaga Z, Różdżyńska A, Palczewska I, Percentile charts of height, body mass and body mass index in children and adolescents in Poland – results of the OLAF study Stand: Med Pediatr, 2010; 7; 690-700
18. Chwałczyńska A, Rutkowski T, Jędrzejewski G, The comparison of the body composition of children at the early school age from urban and rural area in southwestern Poland: BioMed Res Int, 2018; 2018; 9694615
19. Kasperczyk T: Body posture defects. Diagnostics and treatment, 2004, Cracow, Publishing house KASPER
20. Hagner W, Bąk D, Hagner-Derengowska M: Polish Annals of Medicine, 2011; 18(1); 76-81
21. Leszczak J, Drzał-Grabiec J, Rykała J, Characteristics of chosen lower limb anthropometric parameters in non-weight bearing and in weight-bearing conditions in school children: Przegląd Medyczny Uniwersytetu Rzeszowskiegoi Narodowego Instytutu Leków w Warszawie, 2014; 1; 55-61
22. Walicka-Cupryś K, Ćwirlej A, Domka-Jopek E, Development of the longitudinal arch of the foot in 4-6-year-old children before and after 10 months of corrective gymnastics: Advances in Rehabilitation, 2004; 2; 100
23. Głowacka-Mrotek I, Sowa M, Nowikiewicz T, Foot posture in female patients 5 years after breast-conserving surgery: A case-control study: Breast Cancer, 2018; 25; 325-33
24. Pauk J, Ezerskiy V, Rogalski M, The influence of epidemiological factors on the occurrence of flat foot in children: Physiotherpy, 2010; 18(2); 21-27
25. Mikołajczyk E, Jankowicz-Szymańska A, The influence of fitness on feet arching and lower limbs formation in 7-year-olds: Physiotherapy, 2010; 18(2); 10-20
26. Chang JH, Wang SH, Kuo CL, Prevalence of flexible flatfoot in Taiwanese school-aged children in relation to obesity, gender and age: Eur J Pediatr, 2010; 169; 447-52
27. Makarczuk A, Gajda D, The incidence of longitudinal flat feet and its prevention and correction in the opinion of primary school students: Physical Activity of People of Different Ages, 2018; 37(1); 63-72
28. Ziętek M, Machniak M, Wójtowicz D, The Incidence of Body Posture Abnormalities in Relation to the Segmental Body Composition in Early School-Aged Children: International Journal of Environmental Research and Public Health, 2022; 19(17); 10815
29. Riddiford-Harland DL, Steele JR, Storlien LH, Does obesity influence foot structure in prepubescent children?: Int J Obes Relat Metab Disord, 2000; 24(5); 541-44
30. Malden S, Gillespie J, Hughes A, Obesity in young children and its relationship with diagnosis of asthma, vitamin D deficiency, iron deficiency, specific allergies and flat-footedness: A systematic review and meta-analysis: Obes Rev, 2021; 22(3); e13129
31. Dowling AM, Steele JR, Baur LA, Does obesity influence foot structure and plantar pressure patterns in prepubescent children?: Int J Obes Relat Metab Disord, 2001; 25(6); 845-52
32. Ahsan M, Determine the kinematics and kinetics parameters associated with bilateral gait patterns among healthy, overweight, and obese adults: Acta Biomed, 2022; 93(5); e2022228
Tables
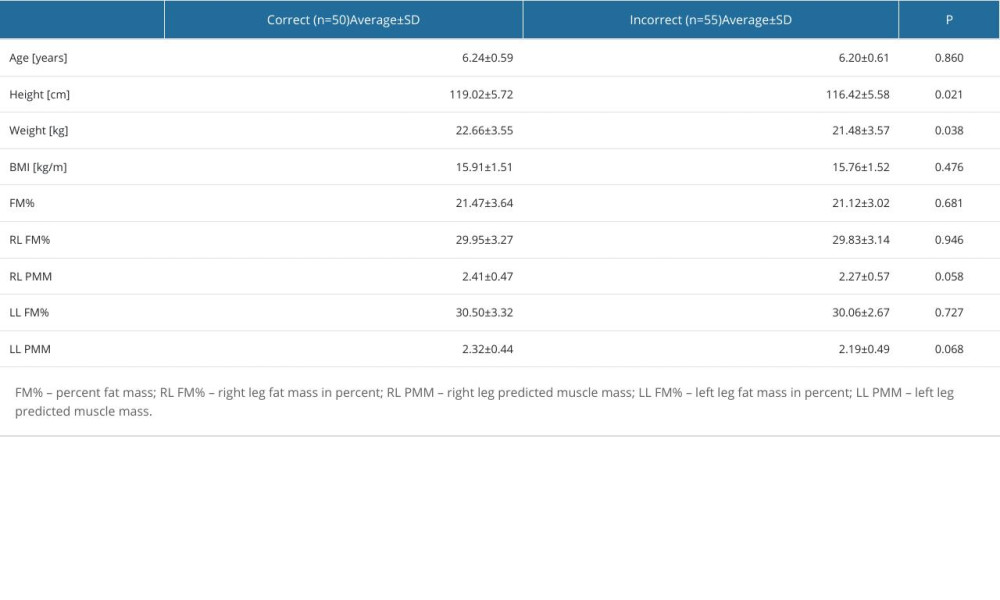 Table 1. Comparison of anthropometric values between the studied groups based on the presence of foot structure abnormalities.
Table 1. Comparison of anthropometric values between the studied groups based on the presence of foot structure abnormalities.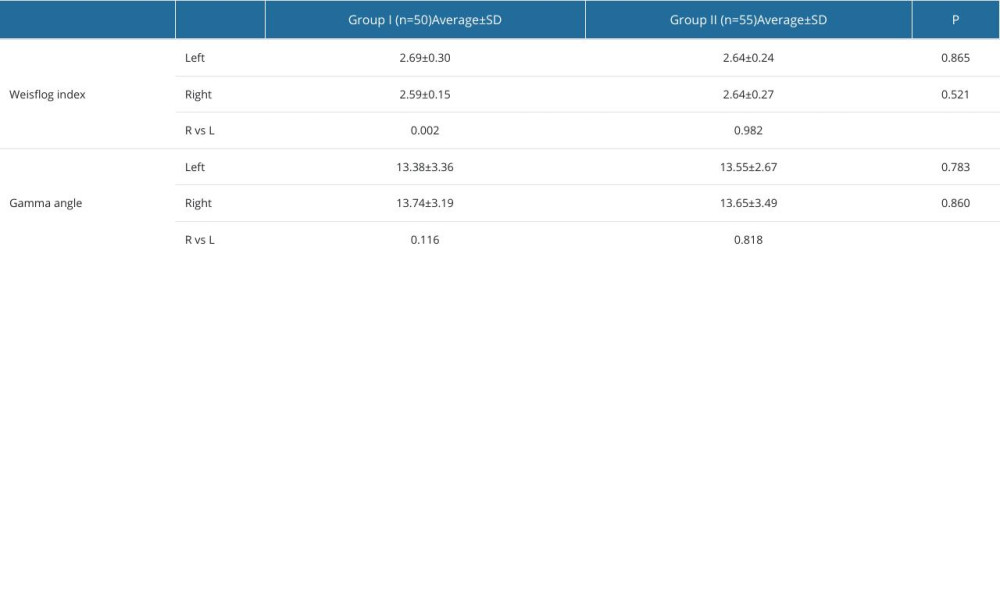 Table 2. Results of calculated Weisflog index and gamma angle.
Table 2. Results of calculated Weisflog index and gamma angle.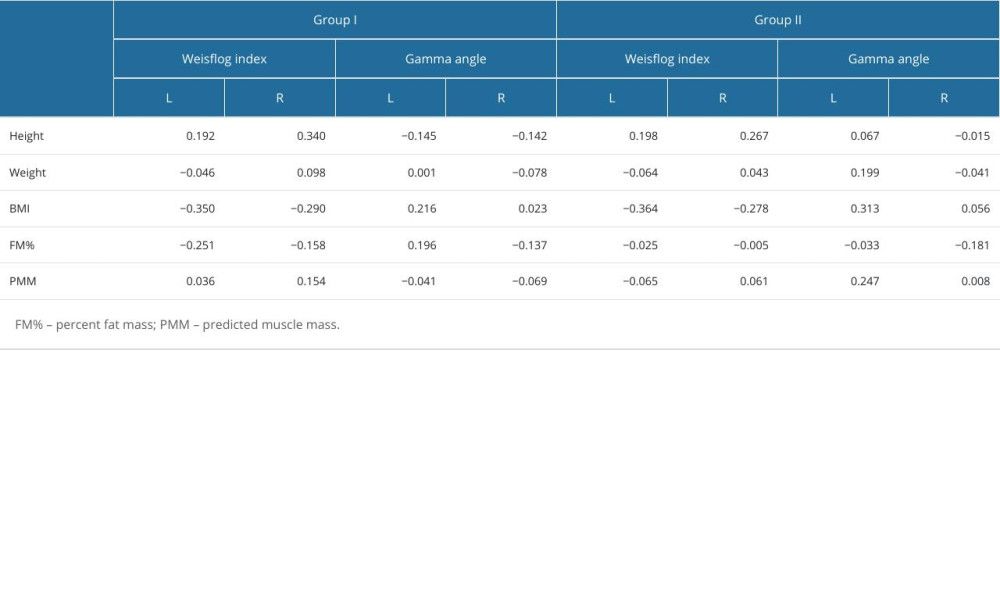 Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.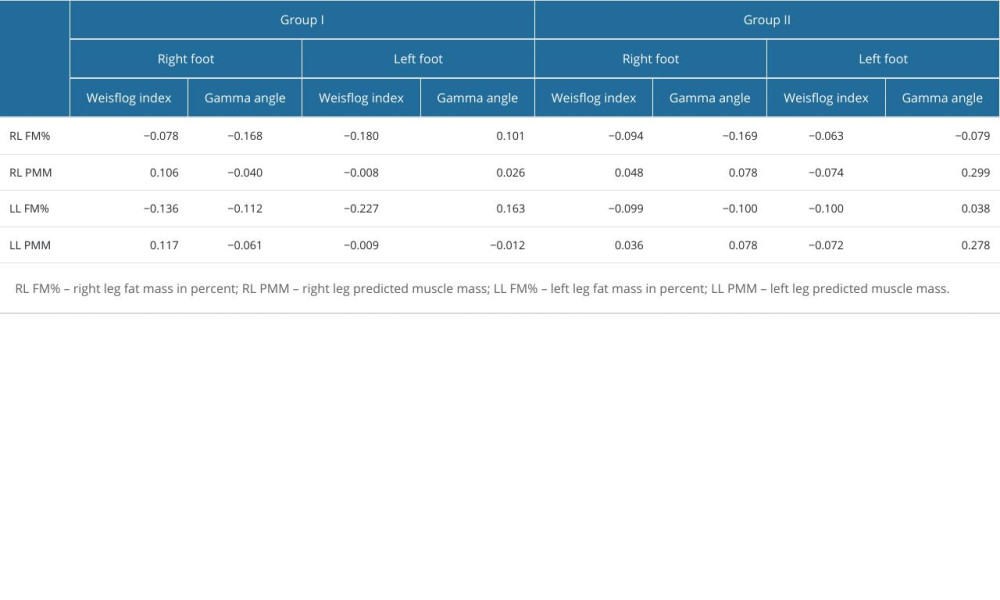 Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.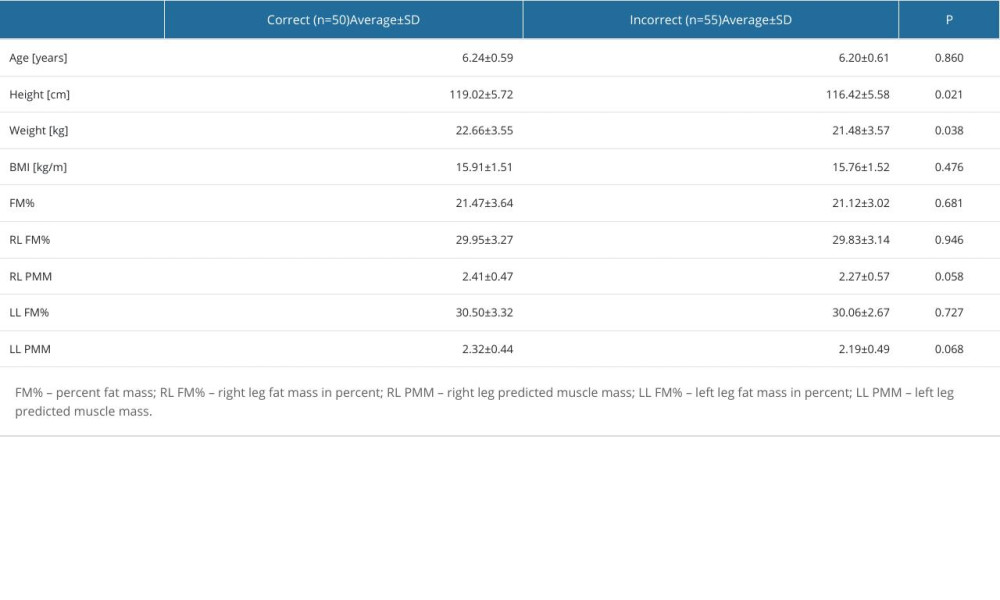 Table 1. Comparison of anthropometric values between the studied groups based on the presence of foot structure abnormalities.
Table 1. Comparison of anthropometric values between the studied groups based on the presence of foot structure abnormalities.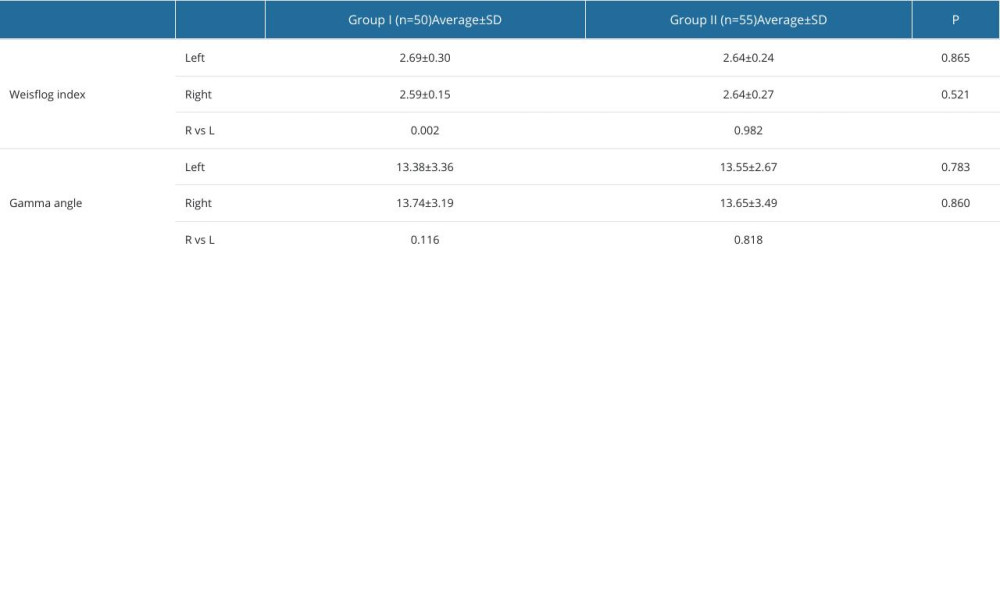 Table 2. Results of calculated Weisflog index and gamma angle.
Table 2. Results of calculated Weisflog index and gamma angle.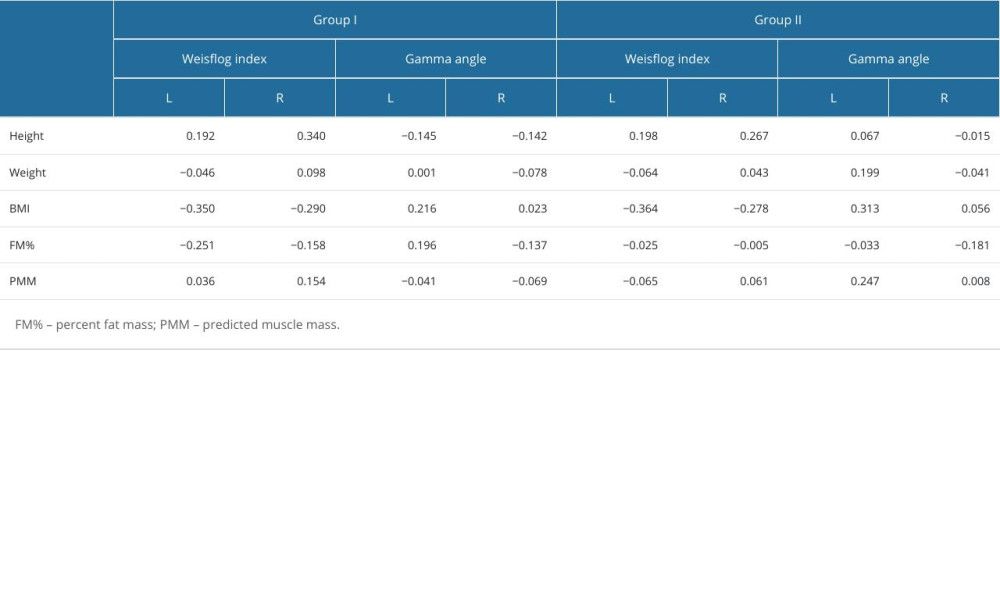 Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 3. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.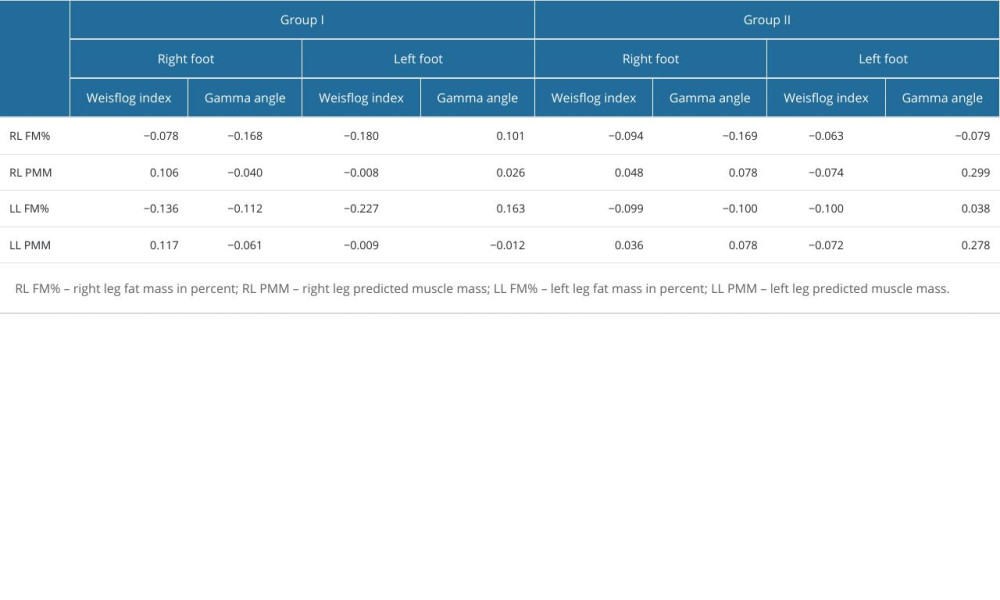 Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet.
Table 4. Correlations between the Weisflog index and gamma heel angle for the right (R) and left (L) feet. In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952