20 April 2024: Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A Retrospective Study of 16 Patients Using Expandable Cages
Hüseyin DemirDOI: 10.12659/MSM.943797
Med Sci Monit 2024; 30:e943797
Abstract
BACKGROUND: Reconstruction surgery using titanium vertebral body replacements aids in spinal stability after damage. Functional evaluation includes Nurick and ASIA grading systems. This study compares outcomes of single and double-level corpectomy in patients treated with thoracolumbar reconstruction.
MATERIAL AND METHODS: Records of 16 patients who underwent vertebral reconstruction with expandable cages after single (n=9) and double (n=8) corpectomy were analyzed retrospectively. Thoracal and lumbar cases were approached posteriorly (n=14). Clinical evaluation was performed by neurological examination, Nurick Scale, American Spinal Injury Association (ASIA) Neurological Scores, and Visual Analog Scale (VAS). Preoperative and postoperative 3-month scores were recorded. Radiological evaluation was performed by calculation of regional angulation and postoperative recovery of vertebral body height.
RESULTS: Preoperatively, 2 patients had no motor or functional sensory deficits (ASIA grade E) and 6 patients were ASIA grade D. Immediately after surgery, 4 of the ASIA grade D patients improved to ASIA grade E, while 2 patients remained ASIA grade D during follow-up. Four patients were ASIA grade A; their conditions showed no improvement postoperatively. Preoperative and postoperative 3-month Nurick grade was statistically significant (P=0.022). Postoperative Cobb angle improved by a mean of 5.4° (P=0.001). Improvement by at least 1 grade in neurological recovery was observed in 6 (38%) of the cases. Pain scores analyzed using the VAS changed from a mean of 7 to a mean of 2.63 (P<0.001).
CONCLUSIONS: In our experience, expandable cages are useful in the restoration of different pathologies of the thoracolumbar trunk with low complication and revision rates. With expandable cages it is possible to achieve restoration of the Cobb angle, improvement in Nurick Grade and effective pain palliation.
Keywords: Spine, Surgical Procedures, Operative, Titanium, Tuberculosis, Spinal, visual analog scale
Introduction
The anterior spinal column can be damaged by primary spinal tumors, metastases, infections, deformities, and trauma [1]. To prevent vertebral body collapse and spinal instability after spinal column damage, reconstruction surgery with stabilization, decompression, single-level and double-level corpectomy, and titanium vertebral body replacement can be used [2]. These titanium grafts consist of 2 telescoping, internally threaded cylinders with wide windows to help pack bone graft material together. Following the corpectomy, the implant’s length is precisely adjusted with optimal in situ distraction using fluoroscopic guidance to accommodate the vertebral defect. Spikes on the cage’s endplates help it dock securely into the nearby vertebral bodies’ subchondral bones. By having a wide axial profile, the cage maximizes the surface area that comes into touch with the vertebral bodies both above and below the operating level. Rather than using an additional apparatus, the cage provides distraction to the vertebral endplates.
There are several measures available to evaluate patients’ functional impairment. One of the most used ones that primarily evaluates ambulatory status is Nurick, which was presented in 1972 for cervical spondylosis [3,4]. The other measure commonly used is American Spinal Injury Association (ASIA), which is a grading and classification system for spinal cord injuries, released in 1982 by the American Spinal Injury Association [5]. In our study, to evaluate the functional disability of patients, we used both the Nurick and ASIA grading.
Single-level corpectomy entails the excision of 1 vertebral body and disc, often used to decompress the spinal cord from large disc herniations or localized tumors. This procedure restores spinal stability and function by replacing the excised vertebral body with bone grafts or implants. Double-level corpectomy involves the removal of 2 adjacent vertebral bodies and discs. It is used for more extensive spinal pathologies such as multi-level degenerative disc disease or expansive spinal tumors. Reconstruction following double-level corpectomy requires larger bone grafts, additional implants, or fusion techniques. This retrospective study from a single center included 16 patients treated with thoracolumbar reconstruction with expandable cages, and aimed to compare outcomes from single-level and double-level corpectomy.
Material and Methods
PATIENT INCLUSION CRITERIA:
Any patient receiving anterior column reconstruction with an expandable cage met the inclusion criteria. Severe mechanical back pain, pathological fractures with >50% loss of height, and >50% vertebral body resection were among the indications for anterior column reconstruction. Patients who did not require anterior column reconstruction were not included.
CLINICAL EVALUATION:
Neurological functional assessment was performed with the Nurick and ASIA impairment scales, preoperatively and postoperatively after 3 months [6]. In Nurick grading, patients with signs or symptoms of root involvement, yet lacking evidence of spinal cord disease, fall under grade 0. Grade 1 indicates the presence of spinal cord disease without hindrance in walking. Grade 2 represents patients experiencing mild difficulty in walking but still able to maintain full-time employment. Grade 3 denotes significant walking difficulty, inhibiting full-time employment or the ability to complete household tasks independently, yet not severe enough to necessitate assistance for walking. Grade 4 marks patients who rely on assistance or walking aids, such as frames, to move. Grade 5 characterizes those who are confined to a chair or bedridden due to the severity of their condition; unable to walk independently [3].
In the ASIA Impairment Scale, the loss of all motor and sensory abilities distal to the site of the lesion, including sacral roots, is referred to as a total spinal cord injury. These injuries are classified as grade A. A partial loss of motor or sensory function below the site of injury is referred to as an incomplete injury. These are ranked B through E. Individuals with lesions classified as grade B have no motor function and partial sensory function. Less than 3 motor grades below the neurologic level of injury characterize grade C injuries, whereas at least 3 motor grades below the neurologic level of injury characterize grade D injuries. Even when the motor and sensory exams of patients with Grade E injuries are normal, the patients may nonetheless exhibit aberrant reflexes or other neurologic abnormalities [5]. Visual Analog Scale (VAS) was used to assess pain [7]. Neurologic status was assessed using the Frankel grading scale.
RADIOLOGIC EVALUATION:
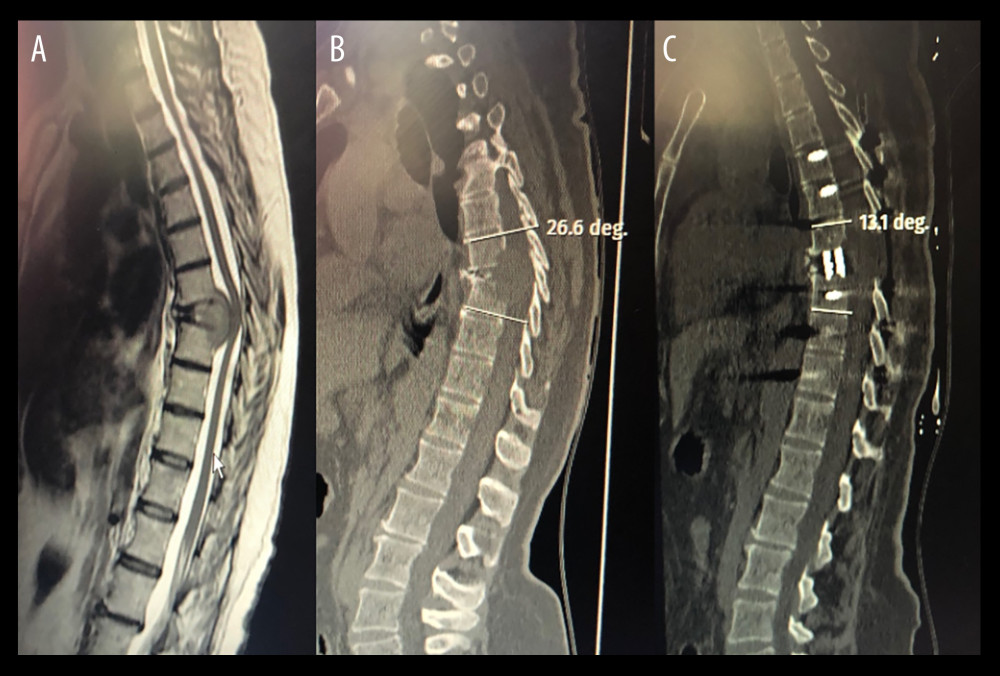
All patients underwent evaluations preoperatively, right after surgery (before being discharged), and 3, 6, and 12 months after surgery. To evaluate the stability and fusion status of the operated section, serial radiographs of the pertinent segment were acquired. After surgery, postoperative CT imaging scans of the affected area were carried out to record the cage and screw locations and to assess the degree of spinal decompression and fusion. Using the Cobb angle, kyphotic deformity was assessed on thoracolumbar spine lateral radiographs. The Cobb angle was measured from the top endplate of the vertebra at the upper level (where the corpectomy was done) to the bottom endplate of the vertebra at the lower level. The kyphotic angle was assessed preoperatively, immediately following surgery, 1 month after surgery, and during the final follow-up appointment (8–28 months; mean follow-up time was 18 months). The lateral radiograph was used to measure the height of the structure as the separation between the lower endplate of the upper and lower vertebrae. Three months following surgery, all patients had dynamic X-ray and CT scans performed to evaluate stability, fusion, subsidence, and potential hardware displacement. It can be difficult to determine fusion when using anterior thoracolumbar instrumentation. If there was no motion on flexion-extension films, zero radiolucency at the junction of the interbody graft and vertebral body, and no indication of an angulation shift in spacing after a follow-up of 1 year, the construct was deemed stable. The mean radiographic and clinical follow-up time was 18 months (range, 8–28 months).
SURGERY:
In 10 cases, thoracoabdominal surgery was conducted, and in 6 cases, retroperitoneal surgery was conducted. To prevent the liver or inferior vena cava from retracting, a left-sided technique was recommended. To obtain an adequate working area for decompression and instrument placement, exposure above and below the diaphragm was necessary in the thoracolumbar approach. Each patient had a corpectomy, the spinal canal was decompressed, and the anterior column was rebuilt utilizing an Alton Sapimed Onspine® cylinder-shaped titanium mesh cage. When preparing the endplates following corpectomy, great care was taken to maintain the bone endplates as much as feasible. The superior and inferior ends of the cage were cut to fit the vertebral endplates’ sagittal alignment. Bone chips containing both demineralized bone matrix as well as synthetic bone as an allograft, particularly in the case of a metastatic spine, were placed within and around each cage, both anteriorly and laterally (Figure 1). In such situations, autograft was taken from the shattered vertebral body and the iliac bone. Iliac bone grafts were utilized to fill the cage in cases of tuberculosis and malignant diseases. To prevent damage to the contralateral segmental vessels, in traumatic instances, the corpectomy was subtotal, leaving a little rim of the vertebral cortex on the other side of the approach. After positioning the plate device, distractive forces were used to lessen the kyphotic deformity.
FOLLOW-UP:
Before the patient was discharged, the clinical examination was carried out in the preoperative and early postoperative phases, and at least 1 year after the surgery. The mean radiographic and clinical follow-up time was 18 months (range, 8–28 months).
STATISTICAL ANALYSIS:
Demographic and clinical variables were analyzed with descriptive statistics. When data conformed to a normal distribution, measurements were represented by the mean and range. Preoperative and postoperative Nurick, VAS, and ASIA scores, as well as angulations, were analyzed with 2-tailed paired
Results
BASELINE AND OPERATIVE PARAMETERS:
Clinical and radiological data for 16 patients were analyzed, retrospectively. Their demographic and clinical characteristics are summarized in Table 1. The median age was 51.7 years (range 24–76). The most common symptom was back pain (87%). A neurological deficit was detected in 62% (10/16) of patients. Four patients had deformities due to Pott disease (25%), and 12 patients had tumors 75%). Three patients had lung cancer, which is the most common tumor etiology.
Thoracal and lumbar cases were approached posteriorly (n=14). The mean follow-up time was 28 months. Two patients had revision surgery due to early complications (1 epidural hematoma and 1 screw malposition), and 1 patient had revision surgery for an L2 burst fracture. Two patients were re-operated 5 and 6 months later, respectively, because of tumor recurrence.
The mean operation time was 5.6 hours (range 5–8). In the thoracolumbar approach, the mean blood loss was 1200 mL (range 800–1700). Surgical complications were observed in 18.75% of the cases. The complications are listed in Table 2. Transient neurological deterioration was seen in 1 case, which occurred after epidural hemorrhage. After detection of neurological damage, the patient underwent revision surgery in 48 hours. In 2 weeks, the patient recovered without permanent deficit.
CLINICAL EFFICACY ASSESSMENT:
Preoperative and 3-month postoperative Nurick and ASIA scores are listed in Table 2. The improvement in Nurick grade was statistically significant (P=0.022). Preoperatively, 2 patients had no motor or functional sensory deficits (ASIA grade E), while 6 patients were ASIA grade D. Immediately after surgery, 4 ASIA grade D patients improved to ASIA grade E, while 2 patients remained at ASIA grade D during follow-up. Four patients were ASIA grade A; their conditions showed no improvement postoperatively. Pain scores were analyzed with VAS, which is listed in Table 2. All patients had pain reduction, which changed from a mean of 7 to a mean of 2.63 (P<0.001).
COMPARING RADIOGRAPHY OF PATIENTS WITH AND WITHOUT EXPANDABLE CAGES:
The difference between mean preoperative and postoperative Cobb angle showed a clear improvement, improving from 16.5 to 10.13, indicating that thoracal kyphosis was restored (
Discussion
LIMITATIONS:
One of our study’s limitations was the limited sample size. A small sample size is insufficient to assess the various results and complications that can arise early or late in cases of surgical treatment such as these. It will take longer-term research (with long-term follow-up) to evaluate the impact of expandable cages over time. Secondly, selection bias may be present since patient pathological examination and surgeon preference play major roles in decision making. Depending on the unique patient’s features, including overall stability, bone quality, and underlying disease, we can decide whether to proceed with further plating or dorsal stabilization. Also, potential biases in information or selection were introduced, and postoperative problems were assessed based on potentially incomplete clinical records. The use of lateral X-ray data to analyze subsidence, and increased CT study of subsidence during and after operations, will be beneficial in future research.
Conclusions
Expandable cages are useful in the restoration of different pathologies of the thoracolumbar spine, with low complication and revision rates. With expandable cages, it is possible to achieve restoration of the Cobb angle, improvement in Nurick grade, and effective pain palliation. Thus, expandable cages are deserving of more study and implementation because they have a promising clinical application future.
References
1. Compagnone D, Cecchinato R, Pezzi A, Diagnostic approach and differences between spinal infections and tumors: Diagnostics (Basel), 2023; 13(17); 2737
2. Rustagi T, Mashaly H, Ganguly R, Transpedicular vertebrectomy with circumferential spinal cord decompression and reconstruction for thoracic spine metastasis: A consecutive case series: Spine (Phila Pa 1976), 2020; 45(14); E820-E28
3. Revanappa KK, Rajshekhar V, Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy: Eur Spine J, 2011; 20(9); 1545-51
4. Nurick S, The pathogenesis of the spinal cord disorder associated with cervical spondylosis: Brain, 1972; 95(1); 87-100
5. Roberts TT, Leonard GR, Cepela DJ, Classifications in brief: American Spinal Injury Association (ASIA) Impairment Scale: Clin Orthop Relat Res, 2017; 475(5); 1499-504
6. Huang H, Young W, Skaper S, Clinical neurorestorative therapeutic guidelines for spinal cord injury (IANR/CANR version 2019): J Orthop Translat, 2019; 20; 14-24
7. Collins SL, Moore RA, McQuay HJ, The visual analogue pain intensity scale: What is moderate pain in millimetres?: Pain, 1997; 72(1–2); 95-97
8. Ruiz Santiago F, Láinez Ramos-Bossini AJ, The role of radiography in the study of spinal disorders: Quant Imaging Med Surg, 2020; 10(12); 2322-55
9. Chen C, Li Q, Wang W, Comparison of the efficacy of expandable interbody fusion cage (EXP-IFC) and non-expandable interbody fusion cage (NE-IFC) in MIS-TLIF for lumbar degenerative diseases: A systematic retrospective study on 62 patients: Front Surg, 2022; 9; 1008171
10. Marchi L, Abdala N, Oliveira L, Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion: J Neurosurg Spine, 2013; 19(1); 110-18
11. Elgafy H, Behrens K, Comparing expandable and static interbody cages in lumbar interbody fusion: J Spine Surg, 2023; 9(1); 1-5
12. Radovanovic I, Urquhart JC, Ganapathy V, Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis: J Neurosurg Spine, 2017; 26(4); 448-53
13. Shen FH, Marks I, Shaffrey C, The use of an expandable cage for corpectomy reconstruction of vertebral body tumors through a posterior extracavitary approach: A multicenter consecutive case series of prospectively followed patients: Spine J, 2008; 8(2); 329-39
14. Metcalfe S, Gbejuade H, Patel NR, The posterior transpedicular approach for circumferential decompression and instrumented stabilization with titanium cage vertebrectomy reconstruction for spinal tumors: Consecutive case series of 50 patients: Spine (Phila Pa 1976), 2012; 37(16); 1375-83
15. Lu DC, Lau D, Lee JG, Chou D, The transpedicular approach compared with the anterior approach: An analysis of 80 thoracolumbar corpectomies: J Neurosurg Spine, 2010; 12(6); 583-91
16. Arts MP, Peul WC, Vertebral body replacement systems with expandable cages in the treatment of various spinal pathologies: A prospectively followed case series of 60 patients: Neurosurgery, 2008; 63(3); 537-45
17. Lu DC, Wang V, Chou D, The use of allograft or autograft and expandable titanium cages for the treatment of vertebral osteomyelitis: Neurosurgery, 2009; 64(1); 122-30
18. Elder BD, Lo SF, Kosztowski TA, A systematic review of the use of expandable cages in the cervical spine: Neurosurg Rev, 2016; 39(1); 1-11
Tables
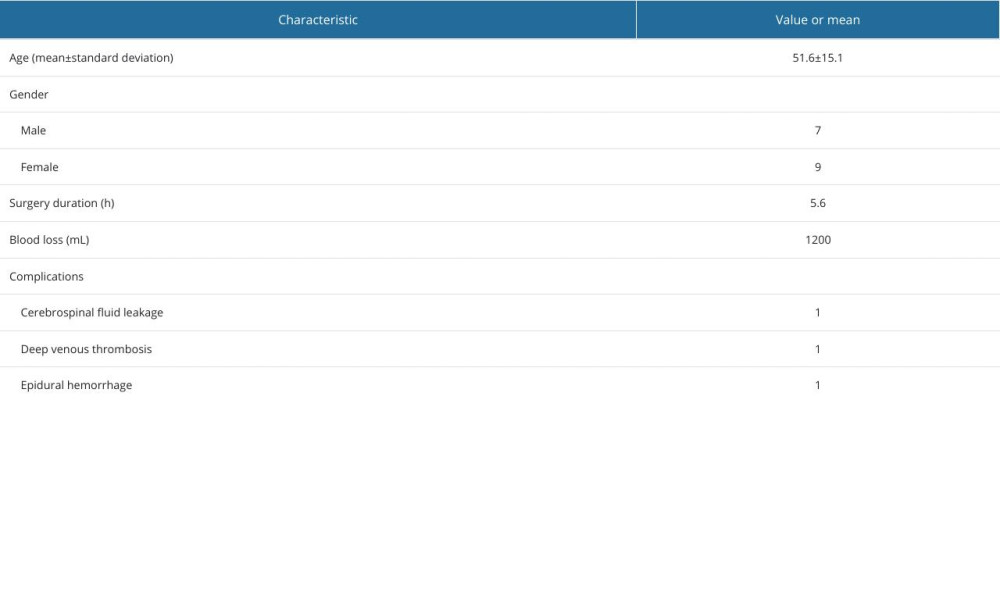 Table 1. Patient demographic and medical characteristics.
Table 1. Patient demographic and medical characteristics.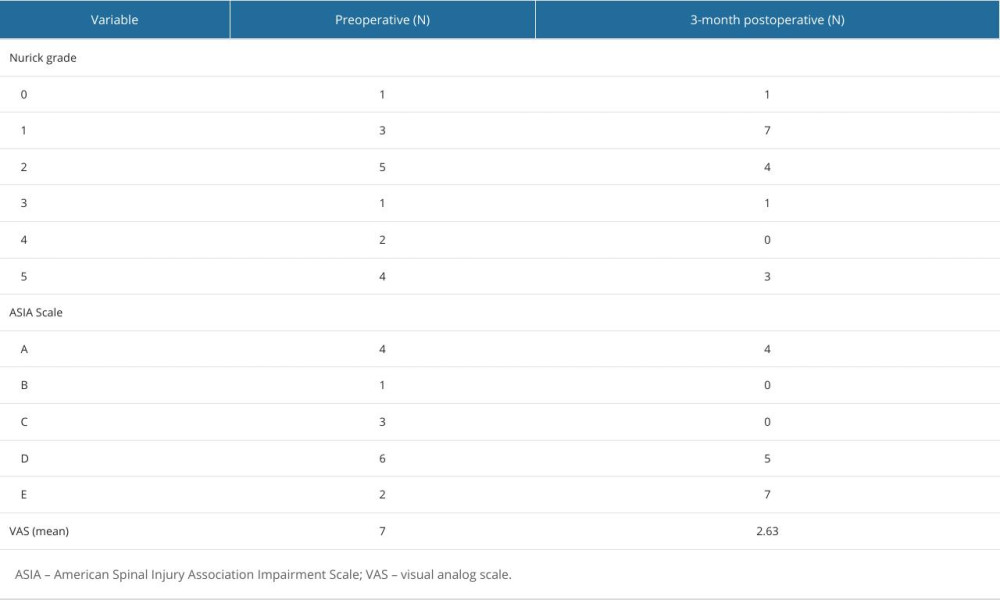 Table 2. Number of patients with clinical characteristics at preoperative and 3-month postoperative assessments: Nurick grade, ASIA scale, and VAS score.
Table 2. Number of patients with clinical characteristics at preoperative and 3-month postoperative assessments: Nurick grade, ASIA scale, and VAS score. Table 1. Patient demographic and medical characteristics.
Table 1. Patient demographic and medical characteristics.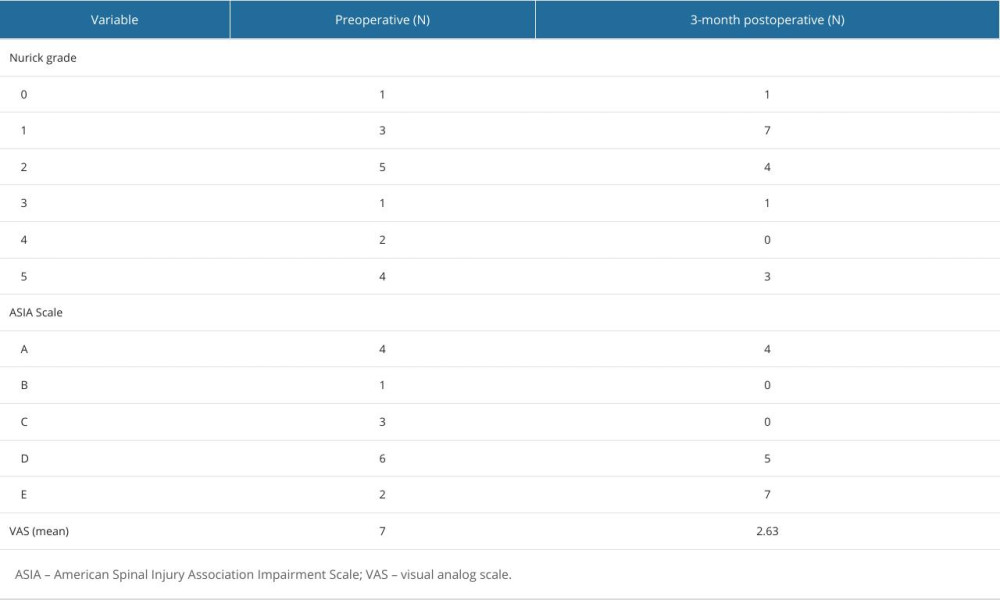 Table 2. Number of patients with clinical characteristics at preoperative and 3-month postoperative assessments: Nurick grade, ASIA scale, and VAS score.
Table 2. Number of patients with clinical characteristics at preoperative and 3-month postoperative assessments: Nurick grade, ASIA scale, and VAS score. In Press
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952