24 April 2024: Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan University
Fareedi Mukram AliDOI: 10.12659/MSM.943884
Med Sci Monit 2024; 30:e943884
Abstract
BACKGROUND: An aged population is susceptible to chronic diseases, which impacts oral surgery treatment procedures. This retrospective study aimed to evaluate the incidence of medical comorbidities in 640 oral surgery patients treated at the College of Dentistry, Jazan University.
MATERIAL AND METHODS: This single-center observational study investigated medical records of outpatients who visited Jazan University Dental College Hospital in a 1-year period (2018-2019). Patients’ clinical and radiographic archives were screened to obtain relevant data. Categorical and continuous variables were expressed in terms of frequency and mean values, respectively. Differences in variables were statistically analyzed using the chi-square goodness of fit and proportional test, with a probability value P≤0.05 considered significant.
RESULTS: Analysis of 640 patient records included records of 300 men and 340 women who underwent oral surgery, of whom 176 patients (27.5%), including 97 men and 79 women, had medical comorbidities. The most common comorbidities were endocrine disease (7.03%), cardiovascular disease (6.71%), respiratory disease (4.53%), and hematological disorders (3.43%). Individual diseases that showed higher prevalence were diabetes mellitus (4.68%), hypertension (3.43%), bronchial asthma (2.65%), and anemia (1.4%). Differences by sex were observed in many individual disorders.
CONCLUSIONS: Outpatients in oral surgery clinics presented a significant variance in the incidence of medical comorbidities, among which diabetes and hypertension were most common. A proper case history is the best preventive measure that helps a surgeon avert medical emergencies and post-surgical complications.
Keywords: Diabetes Mellitus, Heart Disease Risk Factors, Hypertension, Medical History Taking, Medical Records, Tooth Extraction
Introduction
The dental practice has customarily been an independent and isolated affair of treating patients, without giving any regard to their general health. Not until scientific evolution and the development of more sophisticated dental treatment procedures, which can cause considerable stress on the human body, and better definition of medical liability and the duty of care carried by practitioners, have dentists been looking beyond the oral cavity to the comprehensive healthcare of patients. Dental treatment, especially that related to facial aesthetics, is sought by patients, even at an early age. A dentist therefore is in a favorable position to discover an underlying medical comorbidity that may be unknown to the patient. The early comprehensive healthcare concept focused on systemic diseases presenting with oral manifestations as the foremost markers [1], which later were demonstrated to influence wound healing [2], have a strong association with the development of periodontitis [3], acutely exaggerate existing medical conditions [4], and influence patients’ tolerance and compliance to dental interventions [5]. Studies also established that poor oral health has adverse effects on systemic health [6], psychosocial well-being [7], and life satisfaction [8]. Social reforms pertaining to the institution of law brought medico-legal aspects to healthcare, since complex healthcare systems are more prone to cause accidents and complications or make errors while providing medical and dental treatment [9]. With medico-legal issues taking center stage globally, general dental practitioners reluctantly perform complex surgeries in primary and private care settings [10]. The outcome of these refinements brought more onus on the specialists performing treatments, especially oral surgical interventions. Recent legislations not only consider patient safety as a basic right but also command that every healthcare worker, hospital, and even academic organization ensure and comply with patient safety procedures [11]. The perception of causing fairly negligible harm to dental patients (compared with medical treatment) and geographic dental clinic dispersion with lack of communication have been found to be primary reasons for dentistry lagging behind medicine in terms of patient safety [9].
Systemic disorders (comorbidity, medical abnormality, multimorbidity) have been described as true abnormalities or diseases that are generally characterized by deviations from normal functioning [12]. Besides having a significant impact on lifestyle and daily activities [13], a significant portion of medical comorbidities (35%) have been associated with high risk of developing a medical emergency while undergoing dental treatment [14]. Dolan et al reported that in academic dental settings, dental patients whose underlying comorbidities were either poorly controlled, unmonitored, or neglected by either patient or dentist were more susceptible to experience a medical emergency [15].
Comorbidities have varying influences on different dental treatments, and within each treatment option the influence further varies at different stages of treatments. For oral surgical procedures, the medical comorbidities are guided and governed by the health categorization scale of the American Society of Anesthesiology (ASA), which outlines the first 4 relevant groups for oral surgery patients [16]. Barring the first category, all 3 ASA categories include the basis of the type and extent of medical comorbidities, which guide whether the patient should be treated in an outpatient or hospital setting. While ASA category 2 does not affect treatment outcome (eg, hepatitis), extreme precautions need to be taken in infection control procedures to ensure safety of the healthcare workers. In addition, other guidelines are specific to the use of anesthesia and its respective techniques [17]. Patients with comorbidities also have discrepancies in anesthesia outcomes in terms of perioperative events and risk of mortality [18]. Practitioners are expected to assess pretreatment risks through judicious detailed patient interviews rather than by depending on needless medical tests.
Oral surgery requires 3 mandatory treatment phases: preparation, prevention, and management. Prevention is completely based on the application of information derived from a thorough medical history and accordingly alters treatment options, determines adequate surgical techniques, delivers correct and appropriate post-surgical behavior/care instruction and plans in advance for intra/post-surgical complications [19]. Eliciting medical history depends on the nature of the treatment visit, including initial, emergency, elective, continuous care, and periodic recall visits [20]. Medical history must include personal, social, medical, drug, and dental history, with particular emphasis on a patient’s chief concern [21]. The derived information when properly applied enables the oral surgeon to determine whether treatment can influence the patient’s systemic health, and whether the patient’s systemic health can influence treatment; the medical history enables the surgeon to monitor and evaluate patients who are aware or unaware of a systemic condition [22]. Common approaches to elicit history are patient self-reporting or in-depth structured patient interview [23]. Other than the possible risk of developing a medical emergency, medical conditions in oral surgical procedures influence the following: the need for antibiotic prophylaxis in particular systemic condition (cancer, solid organ transplant, kidney failure) [24], altering or stopping of existing drugs (immunosuppressants in auto immune disease, anticoagulants in hyper-coagulopathy states) [25], need for premedication (glyceryl trinitrate in angina) [26], implementation of stress reduction protocol (hypertension) [27], avoidance or limited use of vasoconstrictors in local anesthetics [27], need for intravenous sedation and anesthesia [26], need for medical referral (blood pressure >160/100 mm Hg) [26], need to defer surgery (anemia, acute exacerbation in chronic obstructive pulmonary disease) [10], timing of surgery that is aligned with medical procedure or condition (diabetes, hypertension, cardiac conditions, hemodialysis) [10,28], and identification of threat to dental auxiliaries from contagious infections (HIV, hepatitis B or C, Covid-19) [29].
The current literature has consistently highlighted the necessity of anamnesis and raising the awareness of medical comorbidities of patients and the methods to identify them. It has been observed that younger dentists record the anamnesis of the patient’s medical state less often than do older colleagues [30]. Studies across several nations have provided evidence of a low to high prevalence of health situations among dental outpatients, thereby stressing the need of considering regional population characteristics. A prevalence of low (11.7% in Nigeria [31], 12.2% in Thailand [32], 27.7% in Ireland) [33] to moderate (38% in India [34], 42% in West Indies) [35] to very high (73.7% in Iran [36], 86% in Australia [37]), across different time periods (1991 to 2020) substantiates not only the rising prevalence, but also supports the findings of the estimated proportion of non-communicable disease burden, with an expected increase to 57% by 2020 [38], and possibly sheds a new light on early age affliction of such diseases (below the age of 50 years). Two studies determining medical comorbidity prevalence in dentistry, in periodontal patients, from different provinces of Saudi Arabia also indicate a similar trend from low (10% [n=576] in year 2003) [39] to high (40.21% [n=455] in year 2017) [40] prevalence. Therefore, this retrospective study aimed to evaluate the incidence of medical comorbidities in 640 oral surgery patients treated at the College of Dentistry, Jazan University. The objectives of the study were to collect relevant data on the type and distribution of medical diseases that would serve as an extended database representing the frequency of comorbidities in the Kingdom of Saudi Arabia/dentistry in general and to recommend future clinical and administrative reforms for improving healthcare in an academic dental hospital.
Material and Methods
ETHICS AND STUDY DESIGN:
This retrospective study was conducted by the Department of Oral and Maxillofacial Surgery after study approval by the university’s ethics committee (approval number Reg: CODJU-17171). All patients who visited the Outpatient Department were required to sign a written consent form after registering their personal details at the Outpatient Department. Patients were ensured about the confidentiality of their personal information and treatment data. The data for the study were collected between the second and third quarter of 2018. The research was designed as a single center (dental hospital), retrospective, observational study of the digital medical records of dental patients who visited the Outpatient Department of Oral and Maxillofacial Surgery, College of Dentistry at Jazan University during the academic year 2018–2019. The dental hospital houses 4 main departments, with 12 further subdivisions that house 250 digital dental chairs. It has an annual admission of approximately 100 students and is affiliated with the ministry of education (KSA), while having accreditation by the National Center for Academic Accreditation and Evaluation for regulation of academic quality.
All patients who needed medical referral were governed by a nearby government medical hospital with 24 clinics (3 specialized), 200 beds (31 intensive care unit beds), 34 neonatal intensive care unit beds, and 6 operating rooms, with 7/24 emergency services. The Department of Oral and Maxillofacial Surgery treats all patients during outpatient hours (8 AM to 4 PM). Oral and maxillofacial surgical procedures include minor surgeries, such as extraction of tooth (including impacted and non-impacted permanent third molars), dental implants, dental bone and soft tissue grafts, oral biopsy, oroantral fistula repair, periodontal surgeries, alveoloplasty and alveolectomy, corrective jaw surgeries, and minor pre-prosthetic surgeries (vestibuloplasty, double chin corrections, mandibular reconstruction, bone augmentation, and sinus grafts.
SAMPLE SELECTION:
The sample size was calculated at 95% confidence interval, ±4% precision level, with an estimated proportion of 0.5 and a margin error of 2% for the approximate population size of the area (180 000), which resulted in 599. Since it was anticipated that certain records may have to be excluded, the total sample size was estimated as 640 patients. The required sample for the study (convenient sample) was derived by examining the medical history in the patient files that were entered in the database service clinical and practice management software R4 (Carestream Health, Inc, Rochester, NY, USA), including the radiographic records (Sidexis, Siemens, Bensheim, Germany) of the dental Outpatient Department and written record of the Emergency Department.
At the time of patient registration, the hospital provided each patient with a written healthcare checklist questionnaire to complete and sign. The details were then entered into the system manually and verified in the next appointment during preliminary diagnosis, when patients were interviewed in detail about their medical conditions. Patients were then referred to the appropriate department, based on treatment and chief concern, where they were assigned a student who recorded the medical history and discussed it with his/her supervisor. Two independent researchers were trained based on study criteria, followed by calibration using a structured chart, which included the desired study variables: demographic information including patient ID, sex, age, body mass index, marital status, and smoking, dental hygiene practices, systemic status (past and existing medical conditions), and treatment visit purpose (periodontal, orthodontic, prosthodontic, oral surgery, restorations, endodontic, oral lesions).
Other inclusion criteria were age above 18 years, any sex, detailed medical history of various medical comorbidities collected with a checklist that included cardiac and circulatory, respiratory, hormonal (endocrine), liver, renal/genitourinary, gastrointestinal, neurological, infectious/contagious, and allergic diseases. All files or records that were incomplete, lacked relevant dental/medical information, and had inaccurate/non-legible records, an incomprehensible written record, and records of patients below 18 years were excluded. Identifying patients who underwent oral surgery was determined by a handwritten patient activity monitoring sheet, which was individual for each departmental treatment and was submitted to the receptionist at the end of each clinical session. The details on the sheet were then verified with the digital R4 record. Missing and incomplete patient details were immediately corrected by informing the concerned treating doctor. All researchers followed ethical regulations in maintaining patient confidentiality during recording of the data, which were entered into precoded categories.
MEASURES, DATA COLLECTION, EVALUATION, AND ANALYSIS:
A total of 640 medical records were included in determining the prevalence of medical comorbidities, which included 300 records of male patients and 340 records of females. Each comorbidity was identified at different levels: patient self-reported questionnaire, diagnosis by Department of Oral Medicine, and treatment-related history generated by supervising doctors and their respective students. For each specific medical condition, the relevant tests and their values were noted.
STATISTICAL ANALYSIS:
Data were entered into an MS Excel spreadsheet (Microsoft, Redmond, WA, USA), and after cleaning (elimination of errors), the data were organized for efficient analysis under 11 specific body systems: cardiovascular, endocrine, respiratory, hematological, gastrointestinal, neurological, drug allergy, renal/genito-urinary, dermatological, hepatobiliary, and miscellaneous. This was followed by modelling and analyzing the concerned data according to the study aims and objectives. Data interpretation and visualization was performed using the Statistical Package for the Social Sciences version 20 (SPSS, IBM Corp, Armonk, NY, USA). Coded data were then analyzed to derive descriptive and inferential statistics. Continuous variables are described in terms of average values (means, standard deviations) and/or median with interquartile ranges. The frequency number and percentages were used to express categorical variables. The chi-square goodness of fit test and the chi-square proportional test were used to compare the differences between sexes, depending upon whether the data set compared was a single variable or more than 1 variable. Differences were considered to be statistically significant if
Results
STUDY PARTICIPANT CHARACTERISTICS:
A total of 640 patients (mean age 40.85±8.36 years) included 300 men (mean age 39.84±7.66) and 340 women (41.32±8.14), of which 464 patients (203 men, 261 women) were healthy (mean age 39.23 yrs.) and 176 had medical comorbidities (mean age 44.41 years). The estimated incidence of patients with medical comorbidities was 27.5% (Table 1).
MEDICAL COMORBIDITY INCIDENCE:
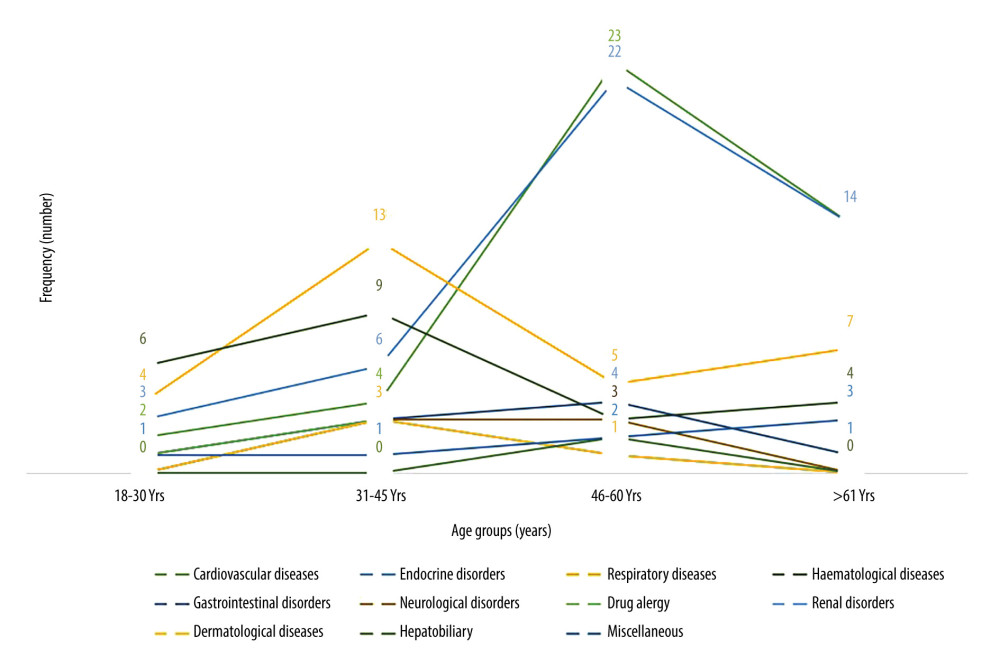
The highest comorbidity type in patients was endocrine disorders (7.05%), followed by cardiovascular (6.71%) and respiratory (4.53%) disorders, while the lowest was hepatobiliary disorders (0.31%). Except neurological and miscellaneous categories (cancer, psychological disorder, immunodeficiencies, nonspecific infections), most patients were men (range 0.33% to 8.67%). For both endocrine and cardiovascular diseases, the mean age of male and female patients was over 50 years. Disorders of hematological, gastrointestinal, genitourinary, hepatobiliary and miscellaneous origin were present in both male and female patients aged between 40 and 45 years (Figure 1). There were marked differences in mean ages between male and female patients for neurological disorders. Among cardiovascular disorders, a higher frequency was observed in hypertension (4.67%), followed by ischemic heart diseases (1.71%), with the lowest prevalence in patients with heart failure (0.15%; Table 2). Hypertension showed a higher predilection toward male patients, while hypotension showed a higher predilection toward female patients, with differences between the two being statistically significant (P≤0.05). Among endocrine disorders, the frequency from higher to lower was diabetes mellitus (4.68%), thyroid conditions (2.18%), and Addison disease (0.15%). Diabetes mellitus was more common in male patients, while thyroid conditions were more common in female patients, with differences for both diseases being statistically significant (P≤0.05). In respiratory disorders, bronchial asthma (2.65%) had a higher prevalence than other respiratory disorders (tuberculosis, chronic bronchitis, emphysema, occupational lung disease, pulmonary hypertension), with all respiratory disorders showing no differences by sex. Among hematological disorders, a higher frequency was observed for anemia (1.40%), followed by sickle cell (0.93%) and bleeding disorders (1.09%). Differences between male and female patients were significant for anemia (women) and sickle cell (men).
Discussion
LIMITATIONS OF THE STUDY:
The study had limitations in its design and methodology. The limitations of design were that it was a single-center, retrospective study that included patients from a single department. The lack of examination or interviewing of the patients was the main limitation of the study design and methods. The chances of missing patient files, incorrect and incomplete files, or files lacking clarity are the major limitations of study methodology.
Conclusions
Within the scope and limitations for this study, it can be concluded that patients with medical comorbidities are an integral part of oral surgery outpatients and that these patients have a higher risk of developing medical emergencies or complications before, during, and after surgical interventions. Patients with medical comorbidities present a varied incidence of diseases, with diabetes mellitus and hypertension most common, which have been reported to affect the delivery and outcome of oral surgical treatment. Recording a detailed case history is a preventive step that should be cultivated among dental students.
References
1. Mohammad SH, Syed KB, Al Harthi SMH, Prevalence of medical conditions among patients visiting dental school in Asir region, Saudi Arabia: A retrospective study: Gulf Med J, 2016; 5(1); 21-26
2. Zandifar E, Sohrabi Beheshti S, Zandifar A, Haghjooy Javanmard S, The effect of captopril on impaired wound healing in experimental diabetes: Int J Endocrinol, 2012; 2012; 785247
3. Rose LF, Steinberg BJ, Minsk L, The relationship between periodontal disease and systemic conditions: Compend Contin Educ Dent, 2000; 21(10A); 870-77
4. Gupta K, Kumar S, Kukkamalla MA, Dental management considerations for patients with cardiovascular disease – a narrative review: Rev Cardiovasc Med, 2022; 23(8); 261
5. Sachdeva SK, Raj SS, Kaushik A, Prevalence of medical problems among patients attending a dental school in India – a cross sectional study: Oral Health and Dental Management, 2015; 14; 429-32
6. Azzolino D, Passarelli PC, De Angelis P, Poor oral health as a determinant of malnutrition and sarcopenia: Nutrients, 2019; 11(12); 2898
7. Yao CS, MacEntee MI, Inequity in oral health care for elderly Canadians: Part 1. Oral health status: J Can Dent Assoc, 2013; 79; d114
8. Ortíz-Barrios LB, Granados-García V, Cruz-Hervert P, The impact of poor oral health on the oral health-related quality of life (OHRQoL) in older adults: the oral health status through a latent class analysis: BMC Oral Health, 2019; 19(1); 141
9. Perea-Pérez B, Labajo-González E, Acosta-Gío AE, Yamalik N, Eleven basic procedures/practices for dental patient safety: J Patient Saf, 2020; 16(1); 36-40
10. Renton T, Woolcombe S, Taylor T, Hill CM, Oral surgery: Part 1. Introduction and the management of the medically compromised patient: Br Dent J, 2013; 215(5); 213-23
11. Kim IS, Park M, Park MY, Factors affecting the perception of importance and practice of patient safety management among hospital employees in Korea: Asian Nurs Res, 2013; 7(1); 26-32
12. Genco RJ, Löe H, The role of systemic conditions and disorders in periodontal disease: Periodontol 2000, 1993; 2; 98-116
13. Al Sweleh FS, Aldhuayan ZM, Alsolaihim NA, Alshamrani HS, Prevalence of medically compromised patients visiting clinics of College of Dentistry at King Saud University: Eur J Pharm Med Res, 2021; 8(2); 158-63
14. Haas DA, Management of medical emergencies in the dental office: Conditions in each country, the extent of treatment by the dentist: Anesth Prog, 2006; 53(1); 20-24
15. Dolan TA, Atchison K, Huynh TN, Access to dental care among older adults in the United States: J Dent Educ, 2005; 69(9); 961-74
16. Sankar A, Johnson SR, Beattie WS, Reliability of the American Society of Anesthesiologists physical status scale in clinical practice: Br J Anaesth, 2014; 113(3); 424-32
17. Lieblich S, Preoperative evaluation and patient selection for office-based oral surgery anesthesia: Oral Maxillofac Surg Clin, 2018; 30(2); 137-44
18. Eyelade O, Sanusi A, Adigun T, Adejumo O, Outcome of anesthesia in elective surgical patients with comorbidities: Ann Afr Med, 2016; 15(2); 78
19. Vettori E, Costantinides F, Nicolin V, Rizzo R, Factors influencing the onset of intra-and post-operative complications following tooth exodontia: Retrospective survey on 1701 patients: Antibiotics, 2019; 8(4); 264
20. Sakr FM, Al-Obaidy KG, Shetty LJ, Formulation of guidelines to resolve medical emergencies in dental practice: An overview: Saudi J Oral Sci, 2016; 3; 3-11
21. Parish CL, Pereyra MR, Pollack HA, Screening for substance misuse in the dental care setting: findings from a nationally representative survey of dentists: Addiction, 2015; 110(9); 1516-23
22. Abraham-Inpijn L, Russell G, Abraham DA, A patient administered Medical Risk Related History questionnaire (EMRRH) for use in 10 European countries (multicenter trial): Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2008; 105(5); 597-605
23. O’Rourke JA, Ravichandran C, Howe YJ, Accuracy of self-reported history of autoimmune disease: A pilot study: PLoS One, 2019; 14(5); e0216526
24. Lopes DR, Peres MP, Levin AS, Randomized study of surgical prophylaxis in immunocompromised hosts: J Dent Res, 2011; 90(2); 225-29
25. Darraj A, Mattoo KA, Nazish M, Scheduling multiple surgical procedures in immunocompromised rheumatoid patient on immunosuppressant regimen: Journal of Medical Science and Clinical Research, 2017; 5(8); 26828-33
26. Woolcombe S, Koshel S, Bryant C, Rood P, Use of intravenous sedation in the management of patients with high blood pressure: Oral Surg, 2009; 2; 116-25
27. National Institute for Health and Care: Excellence Antimicrobial prophylaxis against infective endocarditis, 2008, London, NICE
28. Kumarswami S, Tiwari A, Parmar M, Evaluation of preparedness for medical emergencies at dental offices: A survey: J Int Soc Prev Community Dent, 2015; 5(1); 47-51
29. Mattoo KA, Jain S, Managing prosthodontic (geriatric) patients during the SARS-CoV-2 pandemic: J Int Oral Health, 2020; 12(8); S69-75
30. Čuković-Bagić I, Hrvatin S, Jeličić J, General dentists’ awareness of how to cope with medical emergencies in paediatric dental patients: Int Dent J, 2017; 67(4); 238-43
31. Oyetola EO, Adesina OM, Ogunbameru K, Distribution of medical conditions among dental patients: Niger Med J, 2020; 61(3); 129
32. Dhanuthai K, Sappayatosok K, Bijaphala P, Prevalence of medically compromised conditions in dental patients: Med Oral Patol Oral Cir Bucal, 2009; 14; e287-e91
33. Fenlon MR, McCartan BE, Medical status of patients attending a primary care dental practice in Ireland: J Ir Dent Assoc, 1991; 37(3–4); 75-77
34. Aggarwal A, Panat SR, Talukder S, Self-reported medical problems among dental patients in Western Uttar Pradesh, India: J Dent Educ, 2011; 75(12); 1635-40
35. Al-Bayaty HF, Murti PR, Naidu RS, Medical problems among dental patients at the school of dentistry, the university of the West Indies: J Dent Educ, 2009; 73(12); 1408-14
36. Maryam A, Atessa P, Pegah MM, Medical risk assessment in patients referred to dental clinics, Mashhad, Iran (2011–2012): Open Dent J, 2015; 9; 420
37. Frydrych AM, Parsons R, Kujan O, Medical status of patients presenting for treatment at an Australian dental institute: A cross-sectional study: BMC Oral Health, 2020; 20; 289
38. Shetty A, Nagaraj T, Santosh HN, Shetty N, Determination of medical conditions afflicting patients visiting dental clinics: A population-based survey study: J Adv Clin Res Insights, 2015; 2; 62-66
39. Almas K, Awartani FA, Prevalence of medically compromised patients referred for periodontal treatment to a teaching hospital in Central Saudi Arabia: Saudi Med J, 2003; 24(11); 1242-45
40. Javali MA, Khader MA, Al-Qahtani NA, Prevalence of self-reported medical conditions among dental patients: Saudi J Med Med Sci, 2017; 5(3); 238-41
41. Lakhani MJ, Mehdi H, Kadi W, Girach MM, Comorbidities in patients requiring dental extraction: Pakistan Oral and Dental Journal, 2013; 33; 433-35
42. Alonaizan FA, Almas K, Nazir MA, Medical conditions, oral health practices, and barriers to treatment among patients visiting a Teaching Dental Hospital in Eastern Saudi Arabia: Sci World J, 2022; 2022; 4495757
43. Chandler-Gutiérrez L, Martínez-Sahuquillo A, Bullón-Fernández P, Evaluation of medical risk in dental practice through using the EMRRH questionnaire: Med Oral, 2004; 9(4); 309-20
44. Gaphor SM, Abdullah MJ, Medical status and medication use in patients attending shorish private dental specialty in Sulaimani City: J Interdiscip Med Dent Sci, 2014; 2; 130
45. Sanguansin N, Chinwanitcharoen P, Asavarachan S, Emerged medically compromised conditions in Thai patients visiting a private dental school: World J Dent, 2022; 13(4); 394-99
46. Smeets EC, de Jong KJ, Abraham-Inpijn L, Detecting the medically compromised patient in dentistry by means of the medical risk-related history. A survey of 29,424 dental patients in The Netherlands: Prev Med, 1998; 27(4); 530-35
47. Bhateja S, High prevalence of cardiovascular diseases among other medically compromised conditions in dental patients: A retrospective study: J Cardiovasc Dis Res, 2012; 3(2); 113-16
48. Mesgarzadeh A, Hashemi HM, Sharifi R, A retrospective study of medically compromised patients referred to the Department of Oral and Maxillofacial Surgery, School of Dentistry of Tehran University of Medical Sciences, Iran: J Craniomaxillofacial Res, 2014; 1(1–2); 11-16
49. Siddiqi KM, Baig MZ, Awan MJ, Pattern of medical conditions among patients attending oral and maxillofacial surgery over a period of one year: J Islamabad Med Dent Coll, 2016; 5(1); 26-29
50. Kaur J, Assessing the medical health statistics of patients in a dental institute: J Adv Med Dent Scie Res, 2017; 5(9); 64-68
51. Saengsirinvin C, Kraivaphan P, Phumara P, Survey of drug used and medical history among dental out-patients: J Dent Assoc Thai, 1990; 40; 68-74
52. Umino M, Nagao M, Systemic diseases in elderly dental patients: Int Dent J, 1993; 43(3); 213-18
53. Cottone JA, Kafrawy AH, Medications and health histories: A survey of 4,365 dental patients: J Am Dent Assoc, 1979; 98(5); 713-18
54. Song P, Rudan D, Zhu Y, Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: An updated systematic review and analysis: Lancet Glob Health, 2019; 7(8); e1020-30
55. Catunda RQ, Levin L, Kornerup I, Gibson MP, Prevalence of periodontitis in young populations: A systematic review: Oral Health Prev Dent, 2019; 17(3); 195-202
56. Delavarian Z, Zavar S, An evaluation on patterns and causes of referring patients to oral diseases and diagnosis department of Mashhad dental faculty from September to December 2000: J Islam Dent Assoc Iran, 2004; 16; 62-70
57. Diabetes Atlas, International Diabetes Federation: IDF Diabetes Atlas, 2015, Brussels, Belgium, International Diabetes Federation
58. WHO: Diabetes Country Profiles, 2016, Geneva, Switzerland, World Health Organization
59. Wilson W, Taubert KA, Gewitz M, Prevention of infective endocarditis: guidelines from the American Heart Association: A guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group: J Am Dent Assoc, 2008; 139(Suppl); 3s-24s
60. Lafaurie GI, Noriega LA, Torres CC, Impact of antibiotic prophylaxis on the incidence, nature, magnitude, and duration of bacteremia associated with dental procedures: A systematic review: J Am Dent Assoc, 2019; 150(11); 948-59.e944
Tables
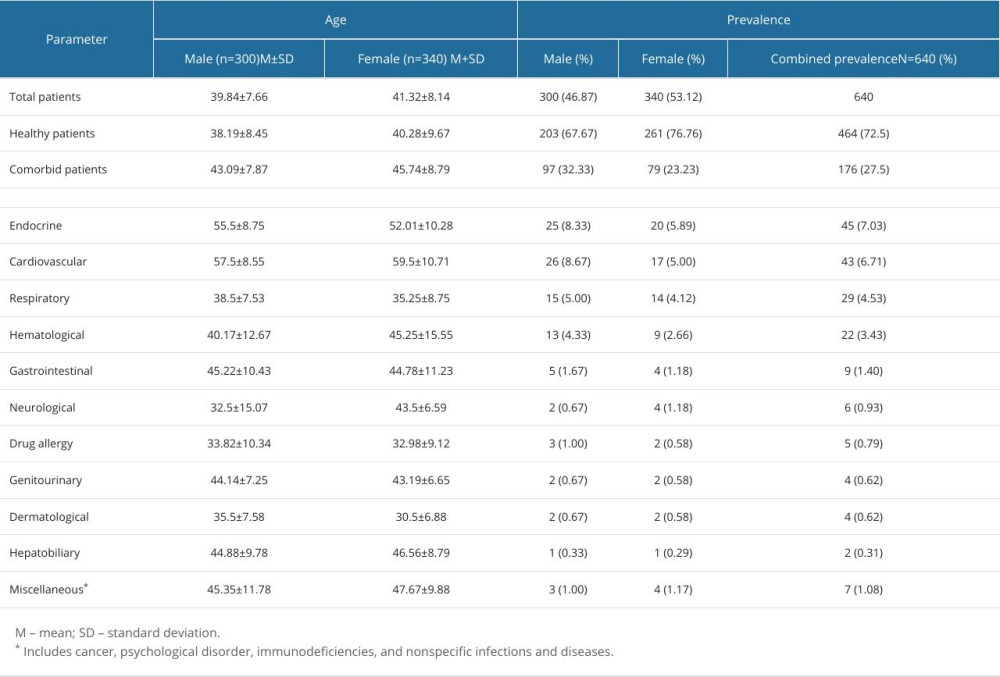 Table 1. Prevalence rates (number and percentage) of healthy patients and patients with medical comorbidities observed during the 1-year time period.
Table 1. Prevalence rates (number and percentage) of healthy patients and patients with medical comorbidities observed during the 1-year time period.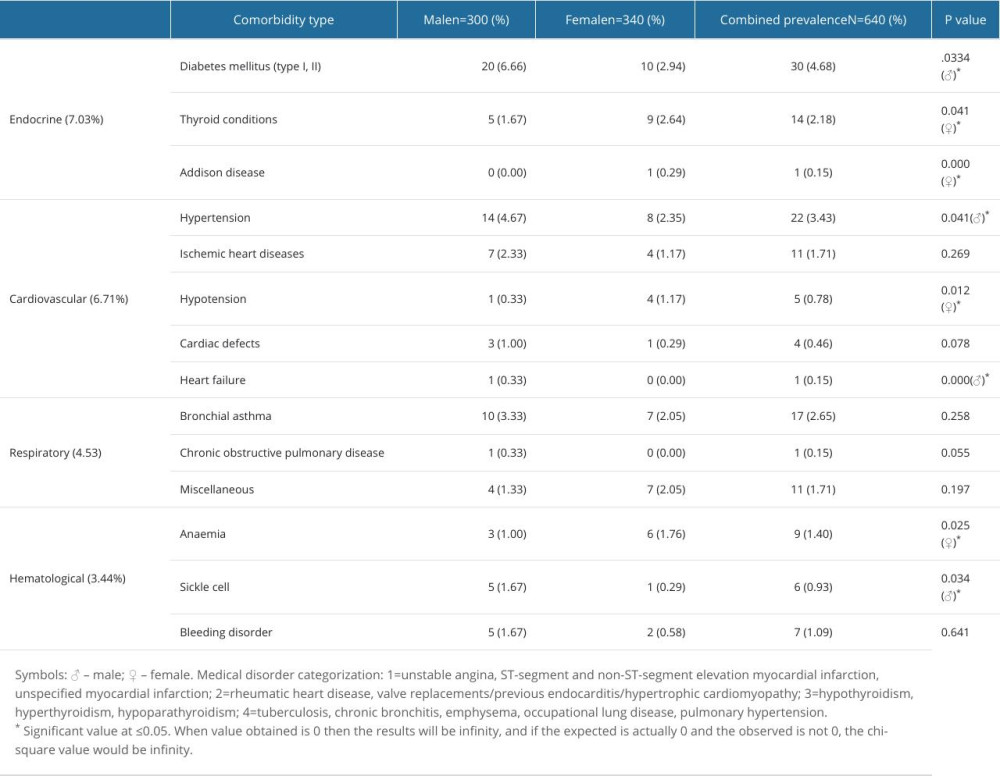 Table 2. Comparative differences in sex in prevalence of 4 commonly encountered medical comorbidities.
Table 2. Comparative differences in sex in prevalence of 4 commonly encountered medical comorbidities.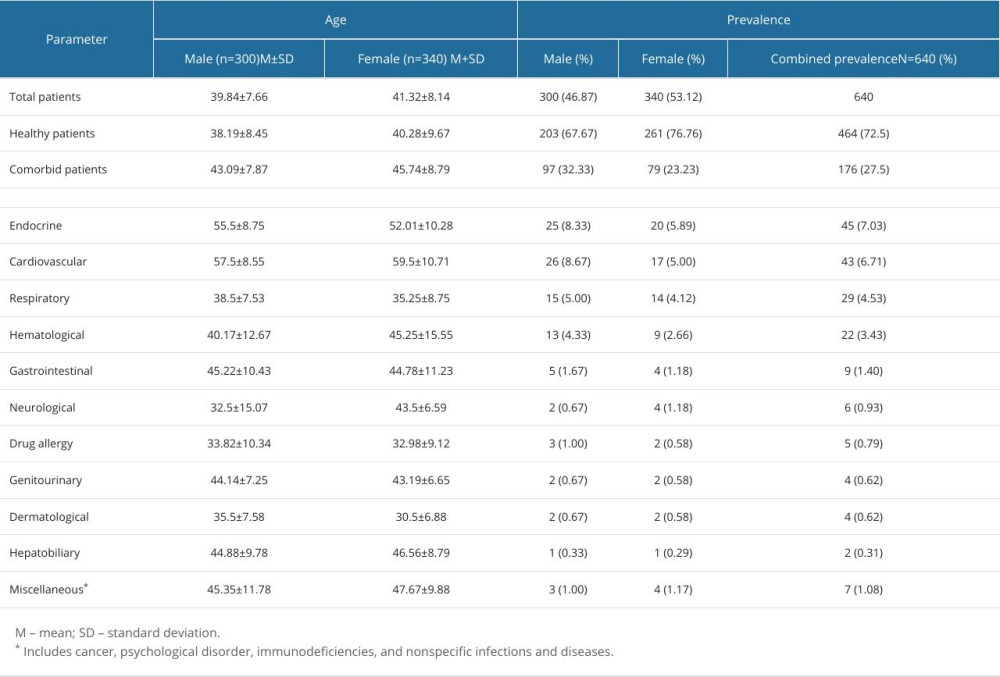 Table 1. Prevalence rates (number and percentage) of healthy patients and patients with medical comorbidities observed during the 1-year time period.
Table 1. Prevalence rates (number and percentage) of healthy patients and patients with medical comorbidities observed during the 1-year time period.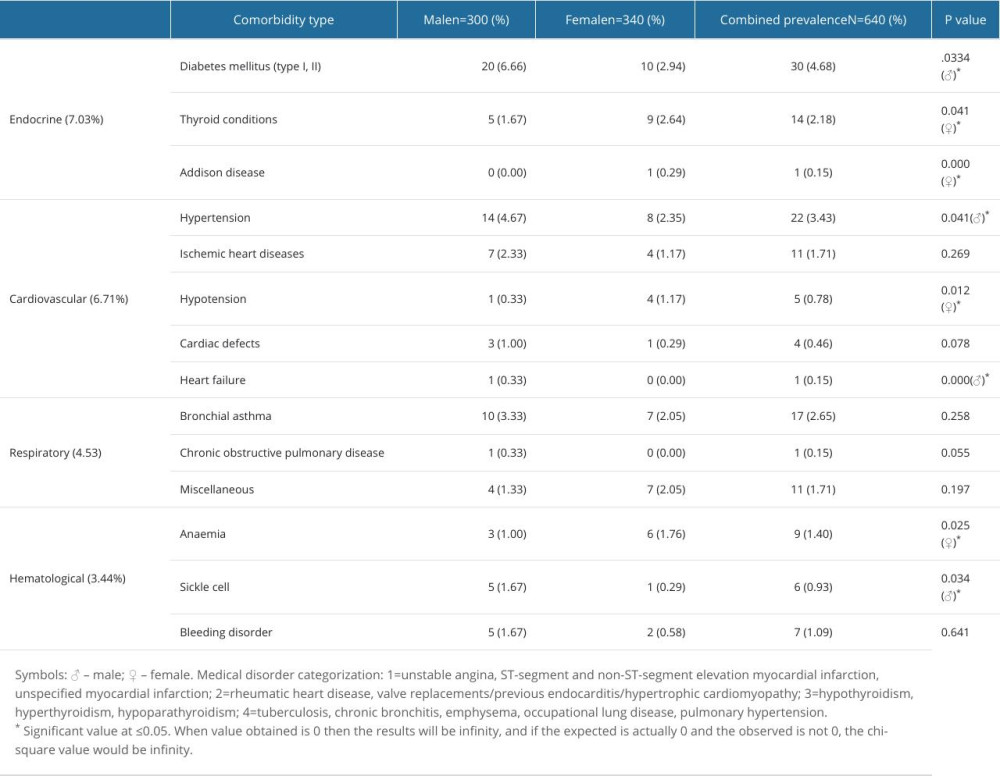 Table 2. Comparative differences in sex in prevalence of 4 commonly encountered medical comorbidities.
Table 2. Comparative differences in sex in prevalence of 4 commonly encountered medical comorbidities. In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952