09 April 2024: Review Articles
A Review of the Current Status of Anesthetic Management of Patients with Rheumatoid Arthritis
Paweł RadkowskiDOI: 10.12659/MSM.943829
Med Sci Monit 2024; 30:e943829
Abstract
ABSTRACT: Rheumatoid arthritis (RA) is a chronic connective tissue disease of immunological etiology. In the course of the disease, symptoms of the musculoskeletal system predominate, but other systems can also be affected. The disease may require long-term treatment, and patients often require surgery on damaged joints. Complications of the disease and drug interactions may contribute to difficulties in perioperative care; therefore, knowledge is required to provide appropriate care. When anesthetizing a patient with RA, we should pay special attention to preoperative evaluation, taking a medical history, risk of difficult intubation or cardiac incidents, respiratory insufficiency, and frequent pulmonary infections. It is important to be aware of perioperative glucocorticoids supplementation, especially in patients with suspected adrenal insufficiency. Postoperative management, such as pain management, early rehabilitation, and restart of pharmacotherapy play, an important role in the patient’s recovery. Special attention should be paid to perioperative management in pregnant women, as the disease is a significant risk factor for complications, and some anesthetic procedures can be noxious to the fetus. Due to the nature of the disease, it can be challenging for the anesthesiologist to provide good and appropriate pain medications, symptom management, and other necessary techniques that are done to anesthetize the patient properly. This work is based on the available literature and the authors’ experience. This article aims to review the current status of anesthetic management of patients with rheumatoid arthritis.
Keywords: Pain, Postoperative, Perioperative Care, Rheumatic Diseases, Arthritis, Rheumatoid, Anesthesia, General
Introduction
Rheumatoid arthritis is a chronic disease of connective tissue; its etiology is still not fully understood. Many factors are considered as potential causes. These include environmental factors (such as viral and bacterial infections – in particular, periodontal infections caused by
RA patients often require orthopedic surgery of damaged joints. Risk factors for surgery include seropositivity, radiographic erosions, and swelling of large joints, whereas negative C-reactive protein is associated with a longer time from RA onset to surgery. Recently, a decrease in the number of operations on small joints has been observed in both sexes, while the number of operations on large joints has remained stable [5,6]. However, in some places the number of foot and ankle surgeries has increased [7].
The disease itself and long-term use of drugs can lead to many problems that an anesthesiologist may encounter. Therefore, patients with rheumatoid arthritis need special attention before, during, and after anesthesia. This article reviews the current status of anesthetic management of patients with rheumatoid arthritis.
Clinical Manifestation of Rheumatoid Arthritis
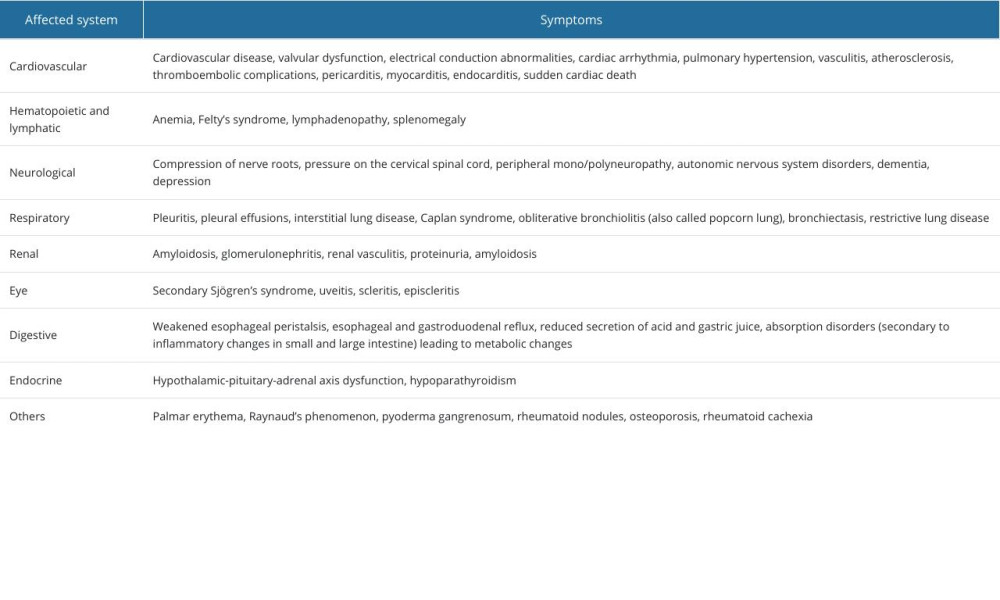
RA is a disease that develops silently over several weeks. Patients can present general symptoms such as low-grade fever, weakness, weight loss, decreased appetite, and muscle pain. Characteristic symptoms include morning stiffness lasting over an hour, swelling, pain, and limited mobility of the affected joints. At the beginning, the disease usually affects the small joints of the hands symmetrically – the proximal interphalangeal joint, the metacarpophalangeal joint, and in the feet, the metatarsophalangeal joint. As it progresses, other joints can also be affected. RA can affect not only the musculoskeletal system but also other systems, causing numerous extra-articular symptoms [1,2,8] (Table 1) [1,9–15].
Treatment
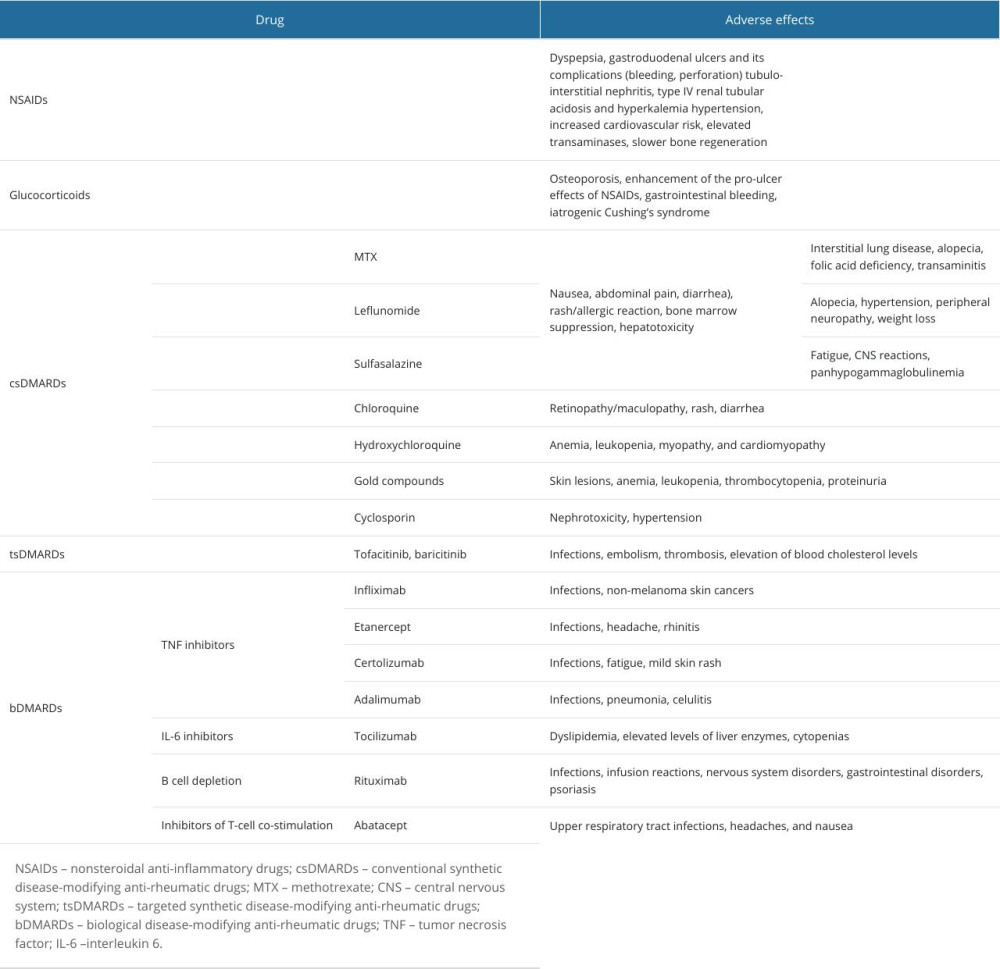
Non-pharmacological approaches (eg, exercise, quitting smoking, physiotherapy, maintaining a normal body weight, and surgery) and pharmacological measures are used in RA treatment. Drugs can be divided into symptomatic and disease-modifying anti-rheumatic drugs (DMARDs) [1,10,15–17]. The first group includes nonsteroidal anti-inflammatory drugs (NSAIDs), which reduce pain and morning stiffness and can increase physical mobility. Glucocorticosteroids enable rapid improvement of symptoms, modify the course of the disease by changing gene expression, and delay the appearance of radiological changes in early stages of the disease, but their use is limited by significant adverse effects that appear during long-term therapy [1]. The second group of drugs, DMARDs, target inflammation in the course of RA, reducing disease activity and severity, improving physical function, and slowing damage; they can be divided into synthetic (conventional (csDMARDs) or targeted (tsDMARDs) and biological (bDMARDs) [1,16]. Methotrexate (MTX) is the most commonly used agent and is considered the criterion standard treatment [1,16,17]. The range of drugs and their multidirectional effects contribute to many adverse effects, as presented in Table 2 [1,10,15,18–23].
Preoperative Management
Preoperative evaluation plays an imperative role in significantly reducing the risks of anesthesia in surgery. Risk factors for surgical complications should be determined (eg, high American Society of Anesthesiologists Physical Status or high Charlson Comorbidity Index) [24,25]. The most common planned surgeries performed on RA patients include reconstructive and repairing joint surgeries, including arthroplasty of hip joints and knee joints, and surgeries on joints of the hands and feet. Patients are usually qualified for elective surgery according to the American Society of Anesthesiologists’ classification for anesthesia as ASA II (mild systemic disease) or ASA III (severe systemic disease that is not life-threatening) [26].
It is important to take a medical history of the exact diagnosis given, any underlying diseases, and disease duration to plan further action, such as choosing the best anesthetic procedure and using an appropriate monitoring technique. It is important to collect a detailed history of medications and comorbidities, perform a clinical examination, assess organ function, and perform additional tests or specialist consultations, if needed. Preoperative discontinuation of DMARDs can exacerbate disease symptoms. Therefore, while planning surgery, the risk of infection due to drug-induced immunosuppression and disease recurrence should be considered [27]. In addition to immunosuppression, smoking and comorbidities also influence the risk of infection [28,29]. In 2022, the American College of Rheumatology and American Association of Hip and Knee Surgeons updated recommendations regarding the suggested time of surgery and the dose of the drug. For patients with RA undergoing elective total hip arthroplasty or elective total knee arthroplasty, it conditionally recommends the following:
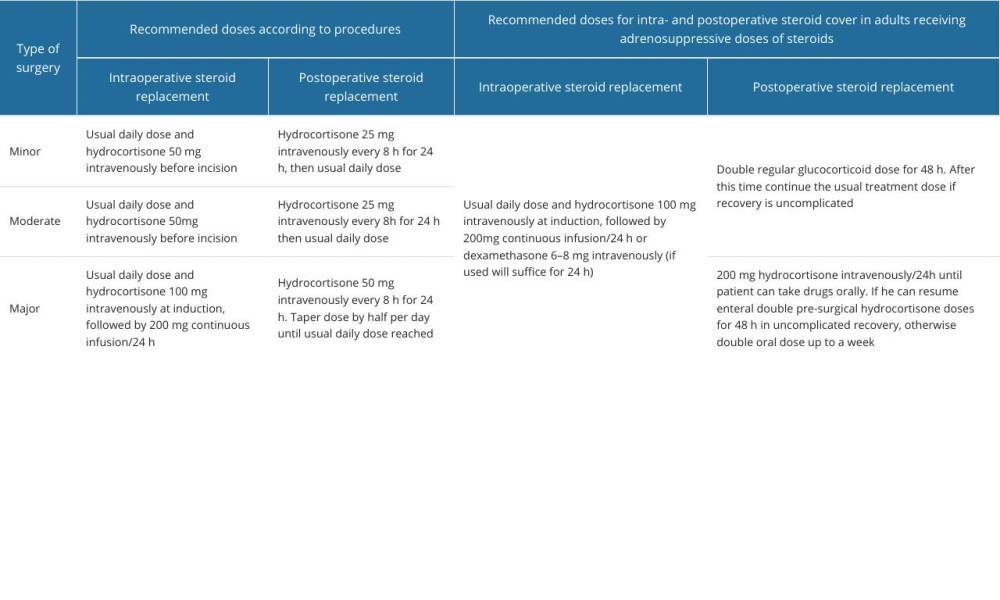
It is conditionally recommended to maintain doses of steroids rather than administering supraphysiological doses on the day of surgery [4,30]. However, additional intravenous hydrocortisone may be needed, depending on the extent of the planned procedure, from 50 mg/day for minor surgeries to 200 mg/day for major surgeries [4]. Guidelines for perioperative supplementation of glucocorticoids were issued by the Association of Anaesthetists, the Royal College of Physicians, and the Society for Endocrinology UK, which are partially presented in Table 3 [4,31,32]. Antithrombotic prophylaxis and discontinuation of anticoagulants should be considered individually in every patient.
Joint changes, bone and cartilage damage, and joint deformations can affect the course of anesthesia, such as causing problems with patient positioning on the operating table, assessment of and access to regional anesthesia, and obtaining vascular access. Therefore, the range of motion in the joints as well as assessment of the rest of the body in terms of deformities and skin lesions should be assessed preoperatively [8]. For anesthesiologists, it is important to perform preoperative clinical assessment and radiological evaluation of the temporomandibular joints and spine joints, in particular the cervical spine and the atlantoaxial and atlanto-occipital joints. Advanced changes in the temporomandibular joints can make it difficult to visualize the entrance to the larynx and to perform intubation. It should be evaluated preoperatively by using the Mallampati score, mandible protrusion, and mouth opening [8,10,33]. In case of difficulty in opening the mouth, especially if the mouth cannot be opened beyond 2 centimeters, video laryngoscopy should be performed for intubation. In case of failed attempt of intubation or if a video laryngoscope is not available, the use of a flexible fiberoptic bronchoscope may be considered [33–39].
Changes in the cervical spine, especially atlantoaxial joint instability, can be caused by even slight head movements, which can lead to compression of the spinal cord, the bulb of the spinal cord, or vertebral arteries, risk of dislocation, and neurological symptoms. Stiffening of cervical spine joints can make intubation difficult or even impossible [10]. Typically, subluxation of the atlantoaxial joint is asymptomatic, so the range of motion (extension and flexion) of the cervical spine should be carefully examined. Magnetic resonance imaging (MRI) improves detection of subclinical atlantoaxial joint subluxation, but the correlation with clinical symptoms is weak and it has no advantage over conventional radiography. However, if neurological symptoms occur, MRI should be considered [4,8]. Subluxation of the atlantoaxial joint is divided into 5 types: anterior (the most common), posterior, lateral, vertical, and subaxial [8].
The cricoarytenoid cartilage can also become inflamed during the disease process. It may be a chronic or acute condition. Clinically, it can manifest as narrowing of the upper respiratory tract, with shortness of breath, hoarse voice, and stridor [8,10]. The larynx is involved in the disease process in 80% of patients. For this reason, preoperative visualization and assessment of the vocal cords and cricoarytenoid cartilage during inspiration using a fiberoptic nasodenoscopy is recommended, but some authors suggest that indirect laryngoscopy before anesthesia be considered [33]. A combination of direct laryngoscopy and computed tomography may be necessary for complete evaluation [8]. In patients with confirmed laryngeal involvement, to minimize tissue traumatization and ensure adequate ventilation, it is recommended to use a small-diameter tracheal tube and, in some cases, perform a preoperative tracheostomy. If general anesthesia is necessary, awake fiberoptic intubation is also recommended [10]. A laryngeal mask airway can be considered as an alternative to tracheal intubation, but there are reports that its use can worsen upper respiratory tract symptoms in people with affected cricoarytenoid cartilage [8,33].
Bilateral cricoarytenoid cartilage involvement in patients with RA is rare but may be life-threatening if it causes airway obstruction and may require emergency tracheostomy [40].
Due to numerous ailments and disorders, and probable difficulties in intubation, and to reduce postoperative complications, the choice of regional anesthesia for both central and peripheral blocks is preferred whenever possible. The use of general anesthesia is associated with a higher incidence of postoperative complications and does not provide sufficient analgesia in the postoperative period [41]. It is believed that assessment for difficult intubation should be performed preoperatively in every patient with RA [42].
Blood Test Results
Both RA and medications taken can contribute to deterioration of the functions of many organs and contribute to an increase in perioperative mortality. Therefore, before surgery, the patient should be carefully examined and the condition of the organs assessed. Hence, the following should be performed: complete blood count, electrolytes, erythrocyte sedimentation rate (ESR), reactive protein C (CRP), arterial blood gas analysis, albumins, complete metabolic panel, blood lipids profile, activated partial thromboplastin time, prothrombin time/international normalized ratio, renal function parameters (creatinine serum level and glomerular filtration rate), urea, rheumatoid factor, and anti-citrullinated protein antibodies [43].
Mild-to-moderate normochromic normocytic anemia is common in patients with active disease and is caused by multiple factors of chronic disease; it can be accompanied with thrombocytosis [44]. These factors include inappropriate level of erythropoietin and a weaker response of cells to it, an increase in pro-inflammatory cytokines, dysregulation of iron metabolism, shorter survival time of erythrocytes, and bone marrow infiltration. In the presence of iron deficiency, microcytic and hypochromic anemia can occur [45]. Low hemoglobin concentration and low body weight in RA patients result in an increased need for perioperative blood transfusion [4,46]. CRP, which is closely correlated with the activity of the inflammatory process, and ESR are commonly used to determine disease activity. The neutrophil-to-lymphocyte ratio may be useful as a marker of disease activity, inflammation, and infection in patients with RA [47]. It is believed that levels of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol, and TC/HDL-C ratio are correlated to some extent with CRP and ESR [48].
Cardiac Risk
RA patients are at risk of increased development of atherosclerosis and cardiovascular disease, especially those with seropositive disease, symptoms of heart failure, poorly controlled disease, and rheumatic cachexia [8,49]. Newly diagnosed patients have a higher risk of developing heart disease and have a higher mortality rate in the event of heart failure (which is major cause of death in RA patients without ischemic heart disease) compared to the rest of the population, despite better blood pressure values and heart function [50]. The cause of sudden death may be cardiac arrhythmia associated with structural changes in the heart – rheumatoid nodules, amyloidosis, and ischemic heart disease [4]. Electrocardiography should be performed and, in the case of symptoms of heart disease or risk factors, echocardiography may be warranted [10].
Pulmonary Risk
The lungs may be affected both by the disease process and as a complication of DMARDs. Patients may experience fibrosis, rheumatoid nodules, and effusion. All patients should have a chest X-ray and, if there is suspicion or history of lung tissue involvement, arterial blood gases and spirometry [8,10].
Intraoperative Management
During the period before the operation and during the operation itself, special attention should be paid to several aspects. Due to the occurrence of osteoporosis, with damage and stiffness of joints, there may be difficulties with properly positioning the patient on the operating table. Therefore, care should be taken when positioning the patient and attention should be paid to support points to avoid pressure sores. Some patients with RA suffer from keratoconjunctivitis, so attention should also be paid to eye protection to avoid corneal ulceration [31]. Patients with RA often have reduced immunity and, as a result, an increased risk of infection; therefore, special care should be taken while applying aseptic principles when establishing intravenous lines or catheterizing the patient [10]. In case of knee surgery, to reduce infectious complications, it may be worth considering the use of sequential pre-disinfection with 2% chlorhexidine on the entire lower limb the evening before the surgery, and 70% alcohol solution 1 hour before the surgery [51]. Intraoperative use of thromboxane (TXA) is recommended – recent studies have shown that patients who received TXA intraoperatively had less blood loss and less need for postoperative blood transfusion compared to patients who did not receive TXA [52].
Anesthetics
The type of anesthesia should depend on the patient’s condition and preferences, the skills of the anesthesiologist, and the type of surgery. As mentioned earlier, whenever possible, regional anesthesia should be preferred. It protects the nervous system against growth afferent nociceptive stimulation occurring during surgery and also persists in the postoperative period, consequently limiting the development of central sensitization and nociceptive stimulation in the postoperative period. Additional advantages of this type of anesthesia over general anesthesia include lower 30-day mortality, reduced frequency of thromboembolism and arterial embolism pulmonary disease, and reduced incidences of pneumonia and respiratory depression [41,53].
For lower limb surgery, spinal anesthesia usually uses local anesthetics with or without an opioid (eg, 0.5% iso- or hyperbaric bupivacaine solution with the addition of fentanyl or sufentanil) [54]. A greater extent of block should be expected, as the sensory block was shown to be 1.5 segments higher than in patients without RA [8]. In some centers, continuous peripheral nerve and plexus blocks (eg, lumbosacral plexus) are used as an alternative to epidural anesthesia. They are useful in orthopedic surgeries, providing good postoperative analgesia and fewer complications compared to general or central neuraxial blocks. However, their use is limited by the fact that the lower limb must be well anesthetized during extensive surgery, because a weak blockade may require the use of general anesthesia, and also by serious complications such as permanent neurological disorders or direct threat to life after intravenous administration of drugs [53,55].
Brachial plexus blocks are used for upper limb surgery from axillary, supraclavicular, or intrascelene access (Winnie’s technique or ultrasonography-guided). The axillary approach should not be used if it is impossible to visualize the needle and its course through a highly vascularized area [56].
Another type of anesthesia that can be considered as an alternative to the previously mentioned ones is intravenous local anesthesia (Bier block), which is a relatively cheap, easy to perform, efficient, and safe type of anesthesia for extremity surgeries of short duration. Serious adverse effects are rare and the most common complication is tourniquet-related pain. The disadvantages of choosing this anesthesia are longer wound healing and the need for additional analgesia after surgery [57]. If general anesthesia is chosen, appropriate airway management devices should be used based on the pros and cons of such a solution. Both safety and the possibility of proper ventilation should be taken into account. As mentioned earlier, special attention should be paid to patients with cricoarytenitis, in whom the aim should be to minimize tissue traumatization and, if possible, supraglottic devices and facemask should be considered; in the case of an endotracheal tube, those with the smallest internal diameter should be selected; in extreme cases, preoperative tracheostomy should be considered. These patients’ extubation should be performed very carefully due to the risk of complications [33].
In patients taking methotrexate, when selecting an anesthetic for general anesthesia, the use of nitrous oxide should be avoided due to the risk of drug interactions [8].
Postoperative Management
Patients with RA require increased attention in the postoperative period. Due to pathologies in the bones and joints, neurological damage may occur perioperatively. Attention should be paid to carefully transferring the patient from the operating table to the bed [8].
Patients with cricoarytenitis, even those without clinical symptoms, are at increased risk of post-extubation edema and require careful observation for respiratory problems, as tracheostomy may be necessary in some cases [8,40]. Patients with RA have a slower recovery and mobilization process after surgery than the rest of the population; therefore, appropriate antithrombotic prophylaxis should be provided. Nevertheless, due to the increased pulmonary risk, attention should be paid to mobilization and breathing exercises as soon as possible [8]. Early rehabilitation shortens the length of hospital stay and the risk of infection [58]. DMARDs should be temporarily suspended in patients who develop symptoms of infection.
They also have an increased risk of peptic ulcers, which is also caused by long-term use of NSAIDs and steroids, so their prevention should also be included in postoperative care [1,8].
An extremely important aspect is ensuring proper analgesia to avoid complications of uncontrolled postoperative pain [8]. Inadequate treatment can delay the initiation of rehabilitation [58]. Due to possible difficulties, pain management teams should be established. The most common method of treatment is pharmacotherapy, but other methods such as multimodal analgesia or regional anesthesia techniques are also used. NSAIDs, due to their inhibitory effect on cyclooxygenase-2, slow bone regeneration and should be used with caution [18]. Opioids, paracetamol, ketoprofen, and metamizole are very commonly used. The use of low-dose ketamine in treatment, which has the effect of supporting respiratory drive, hemodynamic function, and sympathetic tone, has been shown to reduce the need for opioids and the hyperalgesia caused by them [59]. Multimodal analgesia involves the use of a combination of drugs and local anesthetic techniques with different mechanisms of action that have an additive or synergistic effect on various pathways to optimally ensure proper pain control with minimal or even no use of opiates [60,61].
Intensive Care Unit
RA is the most common rheumatoid disease encountered in the intensive care unit (ICU) and the mortality rate of patients suffering from it is relatively high. They are admitted to the ICU due to infections and respiratory failure, and the main cause of death is infection. Patients with rheumatoid diseases in the ICU are at risk of disease relapse or new manifestations of the disease [62]. Predictors of poorer ICU outcomes include: higher Simplified Acute Physiology Score II score, poor health before admission and treated with corticosteroids or immunosuppressive drugs, non-use of csDMARDs, high updated Charlson Comorbidity Index, elevated Acute Physiology and Chronic Health Evaluation II score, and coagulation abnormalities [63]. Patients at risk of heart failure, liver failure, elevated SOFA score, and requirement of vasopressor treatment in the ICU should be promptly identified and treated accordingly [62].
Postoperative Period
The postoperative period is associated with the need to restart pharmacotherapy and return to physical mobility. It is conditionally recommended by the American College of Rheumatology/American Association of Hip and Knee Surgeons that patients who underwent total joint arthroplasty that anti-rheumatic therapy should be restarted once the wound shows evidence of healing, any sutures/staples are out, there is no significant swelling, erythema, or drainage, and there is no ongoing nonsurgical site infection. It usually takes ~14 days [30].
Pregnancy
Most women of reproductive age, with appropriate treatment, can achieve remission or low disease activity, which allows the preservation of fertility and safe pregnancy and childbirth. Women with RA who are pregnant or planning to conceive should be under the care of a multidisciplinary medical team [64]. Patients with active disease have higher risk of preterm delivery and small-for-gestational-age infants. Women with spondyloarthritis have also higher risk of elective and emergency Cesarean delivery and higher risk for preeclampsia [65–69]. During labor and delivery, neuraxial anesthesia should be preferred and general anesthesia should be avoided if possible [70].
Conclusions
RA is a chronic disease affecting many systems, requiring long-term treatment, and contributing to many potential difficulties during anesthetic procedures. Attention should be paid to possible organ complications, difficulties in vascular access, the possibility of difficult intubation, increased risk of infection, and the need for thorough care in the perioperative period.
Patients with RA may require a thorough clinical examination and specific perioperative management. Attention should be paid to perioperative hydrocortisone substitution and dosage depending on the extent of the surgical procedure. Modern technologies enable significant improvement in the preoperative assessment of the patient (eg, imaging tests to determine changes in the atlantoaxial joint), as well as anesthetic procedures such as intubation using a video laryngoscope. Further development of technology, consolidation of available knowledge, and new reports, and linking them with the clinical conditions, are needed to prepare the patient in the best way for surgery and to be able to predict possible adverse effects and counteract them.
References
1. Lin YJ, Anzaghe M, Schülke S, Update on the pathomechanism, diagnosis, and treatment options for rheumatoid arthritis: Cells, 2020; 9(4); 880
2. Chauhan K, Jandu JS, Brent LH, Al-Dhahir MA, Rheumatoid arthritis: StatPearls May 25, 2023, Treasure Island (FL), StatPearls Publishing
3. Batko B, Stajszczyk M, Świerkot J, Prevalence and clinical characteristics of rheumatoid arthritis in Poland: A nationwide study: Arch Med Sci, 2019; 15(1); 134-40
4. Kim HR, Kim SH, Perioperative and anesthetic management of patients with rheumatoid arthritis: Korean J Intern Med, 2022; 37(4); 732-39
5. Richter MD, Crowson CS, Matteson EL, Makol A, Orthopedic surgery among patients with rheumatoid arthritis: A population-based study to identify risk factors, sex differences, and time trends: Arthritis Care Res (Hoboken), 2018; 70(10); 1546-50
6. Asai S, Takahashi N, Asai N, Characteristics of patients with rheumatoid arthritis undergoing primary total joint replacement: A 14-year trend analysis (2004–2017): Mod Rheumatol, 2020; 30(4); 657-63
7. Tominaga A, Ikari K, Yano K, Surgical intervention for patients with rheumatoid arthritis is declining except for foot and ankle surgery: A single-centre, 20-year observational cohort study: Mod Rheumatol, 2023; 33(3); 509-16
8. Samanta R, Shoukrey K, Griffiths R, Rheumatoid arthritis and anaesthesia: Anaesthesia, 2011; 66(12); 1146-59
9. Krishna R, Anjum F, Oliver TI, Bronchiolitis obliterans. [Updated 2023 Aug 14]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK441865/
10. Nkuna AV, Rheumatoid arthritis and anaesthesia: Southern African Journal of Anaesthesia and Analgesia, 2021; 27(6 Suppl 1); S170-74
11. Palomäki A, Palotie AFinnGen Rheumatology Clinical Expert Group, Lifetime risk of rheumatoid arthritis-associated interstitial lung disease in MUC5B mutation carriers: Ann Rheum Dis, 2021; 80(12); 1530-36
12. Kodishala C, Hulshizer CA, Kronzer VL, Risk factors for dementia in patients with incident rheumatoid arthritis: A population-based cohort study: J Rheumatol, 2023; 50(1); 48-55
13. Pedersen JK, Wang L, Risbo N, Mortality in patients with incident rheumatoid arthritis and depression: A Danish cohort study of 11,071 patients and 55,355 comparators: Rheumatology (Oxford), 2023 [Online ahead of print]
14. Kronzer VL, Crowson CS, Davis JM, Trends in incidence of dementia among patients with rheumatoid arthritis: A population-based cohort study: Semin Arthritis Rheum, 2021; 51(4); 853-57
15. Smolen JS, Aletaha D, McInnes IB, Rheumatoid arthritis [published correction appears in Lancet. 2016;388(10055):1984]: Lancet, 2016; 388(10055); 2023-38
16. , Correction: EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update: Ann Rheum Dis, 2023; 82(3); e76
17. Benjamin O, Goyal A, Lappin SL, Disease-modifying antirheumatic drugs (DMARD) [Updated 2023 Jul 3[: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from:https://www.ncbi.nlm.nih.gov/books/NBK507863/
18. Crofford LJ, Use of NSAIDs in treating patients with arthritis: Arthritis Res Ther, 2013; 15(Suppl 3); S2
19. Dunn C, Amaya J, Green P, A Case of iatrogenic Cushing’s syndrome following use of an over-the-counter arthritis supplement: Case Rep Endocrinol, 2023; 2023; 4769258
20. Patel JP, Konanur Srinivasa NK, Gande A, The role of biologics in rheumatoid arthritis: A narrative review: Cureus, 2023; 15(1); e33293
21. Stokkermans TJ, Falkowitz DM, Trichonas G, Chloroquine and hydroxychloroquine toxicity. [Updated 2023 Aug 18]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from:https://www.ncbi.nlm.nih.gov/books/NBK537086/
22. Hoisnard L, Lebrun-Vignes B, Maury S, Adverse events associated with JAK inhibitors in 126,815 reports from the WHO pharmacovigilance database: Sci Rep, 2022; 12; 7140
23. Pflugbeil S, Böckl K, Pongratz R, Drug interactions in the treatment of rheumatoid arthritis and psoriatic arthritis: Rheumatol Int, 2020; 40; 511-21
24. Lee KH, Chang WL, Tsai SW, The impact of Charlson Comorbidity Index on surgical complications and reoperations following simultaneous bilateral total knee arthroplasty: Sci Rep, 2023; 13(1); 6155
25. Sakuraba K, Omori Y, Kai K, Risk factor analysis of perioperative complications in patients with rheumatoid arthritis undergoing primary cervical spine surgery: Arthritis Res Ther, 2022; 24(1); 79
26. Doyle DJ, Hendrix JM, Garmon EH, American Society of Anesthesiologists Classification. [Updated 2023 Aug 17[: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from:https://www.ncbi.nlm.nih.gov/books/NBK441940/
27. Hresko AM, Got CJ, Gil JA, Perioperative management of immunosuppressive medications for rheumatoid arthritis: J Hand Surg Am, 2022; 47(4); 370-78
28. Goodman SM, George MD, Should we stop or continue conventional synthetic (including glucocorticoids) and targeted DMARDs before surgery in patients with inflammatory rheumatic diseases?: RMD Open, 2020; 6(2); e001214
29. Stolzenberg L, Huang A, Usman M, Rheumatoid arthritis-linked artificial joint infections leading to amputations: Cureus, 2023; 15(2); e35622
30. Goodman SM, Springer BD, Chen AF, 2022 American College of Rheumatology/American Association of Hip and Knee Surgeons Guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty: Arthritis Care Res (Hoboken), 2022; 74(9); 1399-408
31. Seo KH, Perioperative glucocorticoid management based on current evidence: Anesth Pain Med (Seoul), 2021; 16(1); 8-15
32. Woodcock T, Barker P, Daniel S, Guidelines for the management of glucocorticoids during the peri-operative period for patients with adrenal insufficiency: Guidelines from the Association of Anaesthetists, the Royal College of Physicians and the Society for Endocrinology UK [published correction appears in Anaesthesia. 2020;75(9):1252]: Anaesthesia, 2020; 75(5); 654-63
33. Gaszyński T, Airway management for general anesthesia in patients with rheumatic diseases – new possibilities: Reumatologia, 2019; 57(2); 69-71
34. Thepmankorn P, Sufian MA, Singer O, Anesthetic implications of previously undiagnosed temporomandibular joint ankylosis: A case report: A A Pract, 2023; 17(1); e01640
35. Moore A, Schricker T, Awake videolaryngoscopy versus fiberoptic bronchoscopy: Curr Opin Anaesthesiol, 2019; 32(6); 764-68
36. Popal Z, Dankert A, Hilz P, Glidescope video laryngoscopy in patients with severely restricted mouth opening – a pilot study: J Clin Med, 2023; 12(15); 5096
37. Alhomary M, Ramadan E, Curran E, Walsh SR, Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: A systematic review and meta-analysis: Anaesthesia, 2018; 73(9); 1151-61
38. Hansel J, Rogers AM, Lewis SR, Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation: A Cochrane systematic review and meta-analysis update: Br J Anaesth, 2022; 129(4); 612-23
39. Yuhono W, Jaya M, Difficult airway intubation due to mouth opening limitation caused by mandibular abscess: A case report. Journal Ilmiah: Kedokteran Wijaya Kusuma, 2023; 12; 193-200
40. Pradhan P, Bhardwaj A, Venkatachalam VP, Bilateral cricoarytenoid arthritis: A cause of recurrent upper airway obstruction in rheumatoid arthritis: Malays J Med Sci, 2016; 23(3); 89-91
41. Ćwiek R, Lisowska B, Małdyk P, The role of the regional anaesthesia performed for orthopaedic procedures in patients with rheumatic diseases: Rheumatology, 2006; 44(3); 145-49
42. Cagla Ozbakis Akkurt B, Guler H, Disease activity in rheumatoid arthritis as a predictor of difficult intubation?: Eur J Anaesthesiol, 2008; 25(10); 800-4
43. Brzustewicz E, Henc I, Daca A, Autoantibodies, C-reactive protein, erythrocyte sedimentation rate and serum cytokine profiling in monitoring of early treatment: Cent Eur J Immunol, 2017; 42(3); 259-68
44. Masson C, Rheumatoid anemia: Joint Bone Spine, 2011; 78(2); 131-37
45. Yilmaz G, Shaikh H, Normochromic normocytic anemia. [Updated 2023 Feb 24]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK565880/
46. Wang X, Zhang L, Li H, Predisposing factors for allogeneic blood transfusion in patients with rheumatoid arthritis undergoing primary unilateral total knee arthroplasty: Front Surg, 2023; 10; 1205896
47. Cui S, Qian J, Future biomarkers for infection and inflammation in rheumatoid arthritis: J Inflamm Res, 2023; 16; 2719-26
48. Lei Q, Yang J, Li L, Lipid metabolism and rheumatoid arthritis: Front Immunol, 2023; 14; 1190607
49. Summers G, Metsios G, Stavropoulos-Kalinoglou A, Rheumatoid cachexia and cardiovascular disease: Nat Rev Rheumatol, 2010; 6; 445-51
50. Błyszczuk P, Szekanecz Z, Pathogenesis of ischemic and non-ischemic heart diseases in rheumatoid arthritis: RMD Open, 2020; 6; e001032
51. Zhang J, Xia C, Zhang J, Wang S, Li J, Sequential pre-disinfection with chlorhexidine and alcohol reduces periprosthetic joint infection after primary knee arthroplasty: A case-control study: Medicine (Baltimore), 2023; 102(47); e36101
52. Wang X, Zhang L, Li H, Predisposing factors for allogeneic blood transfusion in patients with rheumatoid arthritis undergoing primary unilateral total knee arthroplasty: Front Surg, 2023; 10; 1205896
53. Fu G, Li H, Wang H, Comparison of peripheral nerve block and spinal anesthesia in terms of postoperative mortality and walking ability in elderly hip fracture patients – a retrospective, propensity-score matched study: Clin Interv Aging, 2021; 16; 833-41
54. Fonseca NM, Guimarães GMN, Pontes JPJ, Safety and effectiveness of adding fentanyl or sufentanil to spinal anesthesia: Systematic review and meta-analysis of randomized controlled trials: Braz J Anesthesiol, 2023; 73(2); 198-216
55. Lee M, Lee C, Lim J, Comparison of a peripheral nerve block versus spinal anesthesia in foot or ankle surgery: A systematic review and meta-analysis with a trial sequential analysis: J Pers Med, 2023; 13(7); 1096
56. Pester JM, Hendrix JM, Varacallo M, Brachial plexus block techniques. [Updated 2023 Aug 4[: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from:https://www.ncbi.nlm.nih.gov/books/NBK470213/
57. Kraus GP, Rondeau B, Fitzgerald BM, Bier block. [Updated 2023 Aug 5]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK430760/
58. Goto S, Kasuya Y, Okuyama K, Impeding factors of early rehabilitation postoperatively after rheumatoid toe arthroplasty: A single-center retrospective cohort study: JA Clin Rep, 2020; 6(1); 50
59. Allen CA, Ivester JR, Low-dose ketamine for postoperative pain management: J Perianesth Nurs, 2018; 33(4); 389-98
60. O’Neill A, Lirk P, Multimodal analgesia: Anesthesiol Clin, 2022; 40(3); 455-68
61. Helander EM, Menard BL, Harmon CM, Multimodal analgesia, current concepts, and acute pain considerations: Curr Pain Headache Rep, 2017; 21(1); 3
62. Haviv-Yadid Y, Segal Y, Dagan A, Mortality of patients with rheumatoid arthritis requiring intensive care: A single-center retrospective study: Clin Rheumatol, 2019; 38(11); 3015-23
63. Fujiwara T, Tokuda K, Momii K, Prognostic factors for the short-term mortality of patients with rheumatoid arthritis admitted to intensive care units: BMC Rheumatol, 2020; 4(1); 64
64. Tanaka Y, Murashima A, Atsumi T, The management of women of childbearing age with rheumatoid arthritis: An expert report: Expert Rev Clin Immunol, 2023; 19(6); 655-69
65. Andreoli L, Gerardi MC, Crisafuli F, The management of pregnancy in autoimmune rheumatic diseases: analysis of 758 pregnancies from the prospective nationwide P-Rheum.it study (the Italian registry of pregnancy in the rheumatic diseases) abstract OP0125
66. Morin M, Frisell T, Stephansson O, Hellgren K, Are women with spondyloarthritis at increased risk of adverse maternal and infant outcomes? – A Swedish cohort study abstract OP0126
67. Hamroun S, Couderc M, Flipo RM, Unfavorable pregnancy outcome is significantly associated with corticosteroid exposure during pregnancy in women with rheumatoid arthritis abstract OP0127
68. Zucchi D, Racca F, Tani C, Adherence to medications during pregnancy in systemic autoimmune disease abstract OP0128
69. Sim BL, Daniel RS, Hong SS, Pregnancy outcomes in women with rheumatoid arthritis: a systematic review and meta-analysis: J Clin Rheumatol, 2023; 29(1); 36-42
70. Rajagopalan S, Rheumatoid arthritis in pregnancy: Consults in Obstetric Anesthesiology, 2018, Cham, Springer https://doi.org/10.1007/978-3-319-59680-8_137
In Press
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952